Introduction
Experiences of pregnancy and early parenting have been significantly impacted by the global COVID-19 pandemic. Parental anxiety, disruptions to both antenatal care and birth services, and limitations on postnatal support services raise concerns around mental health, infant outcomes, and early parenting. Pregnancy during the pandemic has raised parental concerns about potential harmful effects on foetal development and neonatal outcomes, including concerns around case reports of preterm delivery in COVID-19 positive mothers (Brooks, Weston, & Grenberg, 2020). Central to parental anxieties are experiences of uncertainty as knowledge remains limited, raising existential questions about the future a child may face, given the pandemic’s impact on economic and social functioning, and disruption to daily life. Some question their own capacity to protect a vulnerable infant in the face of health and social risk which constitutes a fundamental threat to the parental role (Preis, Mahhaffey, Heisleman, & Lobel, 2020). These anxieties may be contributing to reported decreases in birth rates in some countries as families choose to delay pregnancy.
Importantly, many reports document increased rates of depression and anxiety during pregnancy and the postnatal period during the COVID-19 pandemic (Farrell, Reagu, Mohan, & Elmidany, 2020; Berthelot et al., 2020). High levels of anxiety in pregnancy raise concerns about the impact of stress-related hormones on foetal development and birth with the known association of maternal anxiety with premature delivery and poor neonatal outcomes. Parental anxiety may relate to fears of contracting the virus and fears that this may harm the foetus (Corbett et al., 2020).
In a prospective study of pregnant women during the pandemic, 50% and 47% reported fears of preterm delivery and foetal structural anomalies, respectively (Thapa et al., 2020). These and related findings raise concerns about the impact of anxiety on the development of the attachment relationship in the antenatal period and potentially on the quality of early interaction with the infant who is seen as vulnerable.
For some parents, having conceived an infant during the COVID-19 crisis creates feelings of guilt and anxiety about ‘bonding’ with the infant in case of poor outcome and loss (Beresic, 2020). These findings raise significant concerns about the mental health of the mother and families during pregnancy, as well as concerns about the impact of maternal stress and mood on foetal development. This increase in distress and psychiatric symptomatology in the antenatal period would, in more normal circumstances, would be the focus of further assessment and intervention aimed at supporting the transition to parenthood, including the development of antenatal attachment, with the addition of postnatal follow-up and support, and a focus on the parent-infant relationship.
The reduction in face-to-face services and usual programs of community-based support during the COVID-19 crisis has contributed to parents experiencing an overall lack of support and social isolation, and many do not have access to their usual extended family support or social networks. In Melbourne, the severe lockdown and lack of movement in the community, has further isolated many vulnerable population groups without traditional family and social support. In turn, this has had specific negative effects on minority cultural groups and those with pre-existing social disadvantage and traumatic experiences, such as asylum seekers and refugees.
The BEAR (Building Early Attachment and Resilience) parent-infant group program described below has been developed to provide infant-parent attachment focussed psychotherapy as a group intervention for parents and families with vulnerability and risk factors, for early parenting difficulties and attachment problems. This is an approach aimed at building parental capacity to reflect on the inner world of the infant and to encourage emotionally attuned interactions and sensitivity. Offered previously as a face-to-face program, BEAR has been delivered to over 100 mother-infant dyads and is currently being evaluated in terms of longitudinal infant outcome and interactional variables (under review).
A major challenge for clinical infant mental health services is to reach vulnerable and isolated families where a combination of psychological and social factors, impacts parenting capacity and increases the risk of early relational trauma with implications for infant psychosocial, and cognitive development. Whilst there are some examples of online and videoconferencing support groups for parents and infants (Marshall et al., 2020), at the time of writing of this article, we are not aware of reports of therapeutic programs used for high-risk infants which are subject to evaluation.
Anecdotally, there has been an increase in the use of parenting support telephone advice services with a reported increase in calls relating to parenting stress, depression, and issues related to family conflict (PANDA, 2020). In this context, we adapted and implemented the BEAR program maintaining the key components and adding the focus on the current pandemic crisis and its impact on both mental health and early parenting. A key issue was identified as the need to build social support and connection for isolated parents, to share experiences and anxieties raised in this situation, and to contain parental anxiety to allow a place to reflect on the needs of the infant for connection and interaction. These are fundamental elements of infant-parent interventions, now adapted for unusual and challenging circumstances.
Significance of the BEAR Program model
The Building Early Attachment and Resilience (BEAR) program is an accessible therapeutic parent-infant mental health program, specifically designed for vulnerable parents. The BEAR program is based on the extant body of evidence about the critical importance of early care and the quality of the parent-infant attachment relationship for infant neurological, cognitive, emotional, and social development (Russo, Murrough, Han, Charney, & Nestler, 2012). Infant brain growth and emotional development are shaped by early experiences of emotional interaction with the parent and the parent’s capacity to support the infant to manage anxiety and self-regulation (Newman, Sivaratnam, & Komiti, 2015).
Importantly, the quality of early emotional interaction and regulation is related to the parent’s/caregiver’s capacity to think about the inner world of the infant and to read, and respond, to infant affective communication. The tasks of establishing a positive relationship with the infant may be negatively impacted by a broad range of caregiver risk factors including maternal anxiety, depression, mental illness such as psychosis, unresolved issues related to early child abuse and neglect, and psychosocial risks including poor social support, experiences of conflict, and family violence (Schore, 2010).
Early intervention services are central in better identification of vulnerable parents and in the provision of timely treatments for perinatal mental disorders and support for the promotion of sensitive emotional interaction and organisation of the attachment relationship with the infant. Available models support the importance of better recognition of the early risk factors for mental disorders and the specific negative impact of stress and trauma on early brain development (Newman, 2015). Early identification and intervention are crucial given the known developmental sequelae of attachment anxiety and early relational trauma, such as vulnerability in later life to the range of mental health disorders and psychosocial disadvantage (Granqvist et al., 2017; Madigan et al., 2019). Early interventions focused on parenting and parent-child relationship quality to optimise child development and to promote psychological resilience and mental health (Slade et al., 2019) while reducing the economic and social burden of untreated attachment-related disorder, issues across the lifespan (Oates, 2007).
The BEAR program is designed to provide vulnerable parents with increased knowledge and understanding of the emotional and social needs of the infant and an understanding of infant communication (Newman, 2012, 2015, 2019). Parents with risk factors for attachment difficulties, including individuals with complex trauma and/or psychopathology, are supported in developing sensitivity to infant communication and to strengthen their role as an available attachment figure. This involves supporting parents to focus and reflect on the emotional communication of their infant and to build an understanding of their infant’s needs, in the relationship. The program addresses parental anxiety, issues related to mood, past trauma, and provides direct clinician-led coaching of interaction with young infants.
The BEAR sessions include three components: (1) Reflection on the parental self, (2) Emotional interaction and building a model of the communication with the infant, and (3) Psychoeducation about attachment and the development of infant’s subjectivity. The program is multidisciplinary and aims to provide both developmental and interactional guidance, maternal and child health nurse support, and parent-infant psychotherapy. The group setting provides social support and apprentices for the sharing of experiences. The weekly schedules and modules of the BEAR program are presented in Table 1.
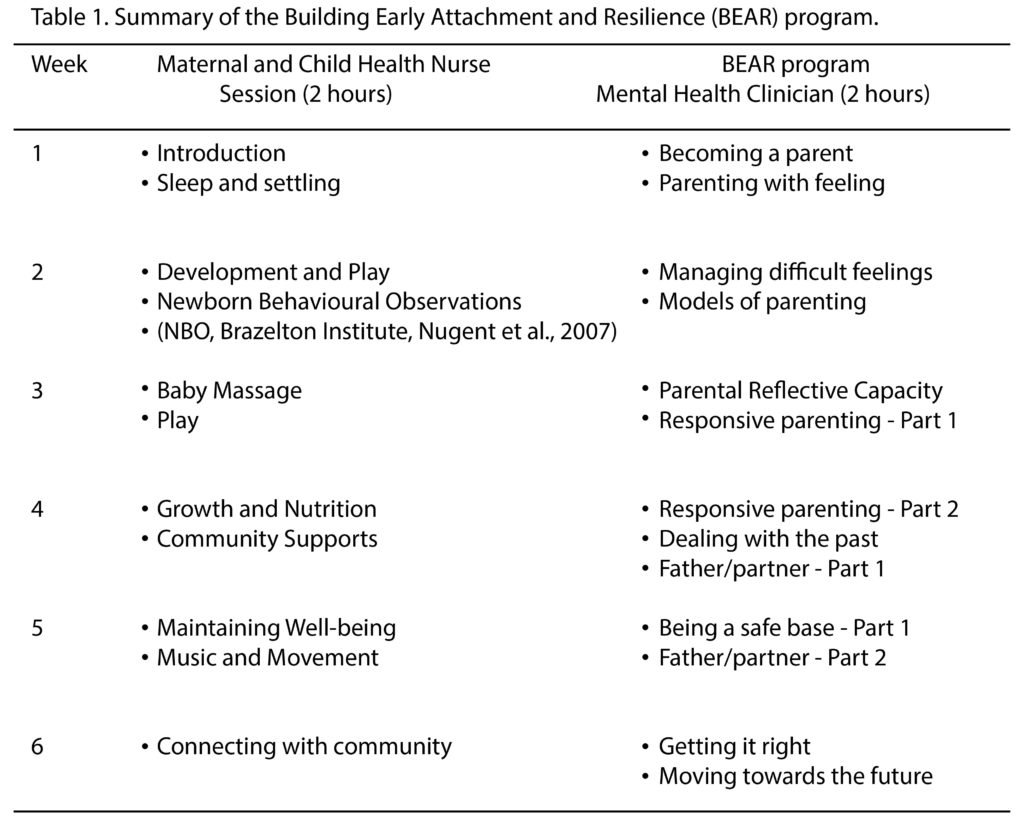
The BEAR program has been adapted and delivered across multiple modalities including in hospital settings working with infants as early as 4-weeks-old, for drug and alcohol using mothers (ABC-WADS program), and as an intensive day community-based program, known as BEAR House. While the majority of the programs are delivered as a 2-hour weekly program, the intensive BEAR House program also includes a maternal and child health component, focused on practical and embodied aspects of parenting such as play, baby massage, information about nutrition, and community engagement (see Table 1 above). Sessions are typically co-facilitated by a psychiatrist/clinical psychologist and maternal and child health nurse/clinician. It is the BEAR House program that was urgently adapted to virtual ACCESS BEAR, due to the necessity in continuing to deliver the service in the face of the COVID-19 pandemic.
Adaptation to ACCESS BEAR during the COVID-19 pandemic: Participant and clinician reflections
In March 2020, a group of 5 mother-infant dyads were attending the community-based BEAR House program delivered face-to-face in Melbourne, Australia. The call of the COVID-19 pandemic public health crisis led to the immediate withdrawal of clinical group services which meant that we had to rapidly adapt the BEAR program to ACCESS BEAR to be able to deliver the rest of the program (two sessions) online to these 5 mother-infant dyads. Participant feedback and other data were collected in the context of broader research study protocol resulting in a unique set of insights about qualitative differences regarding online versus face-to-face treatment modalities. In this group of participants, common reflections regarded the positive aspect of ongoing social connectedness during imposed restrictions and social distancing from extended families and early parenting community services.
Participants also reflected on the comfort and the convenience of having the program virtually delivered to their homes which meant that the practical infant care such as feeding, changing, and sleep remained uninterrupted. However, some participants focused on the loss of face-to-face contact. For example, one mother highlighted:
[it was positive that] we could still have some contact given that at the moment, social distancing would have otherwise made it fairly impossible …though I don’t think the online sessions are as good…you know…’cause [facilitator] mentioned that maybe the next group would have to be run entirely online…personally, having experienced both ways of delivery I personally don’t think I would’ve gotten as much out of attending the program if it was just online because a big part of what I enjoyed about the program was actually interaction with the other mothers and babies as well…it’s a very warm environment…and umm…also the kind of care … [facilitator]…being in person…there is something really special about the way they provide care…
Reflections from this group also included grief about the loss of informal conversation during tea breaks and face-to-face contact for babies. Balanced reflections on grief and loss (i.e. not distorted or preoccupying in form) may be seen as an attempt of the psyche to ingrate the environmental changes and to adjust to the parenting role, and the new circumstances under attachment-related stress (Main, 2000). Notwithstanding the sadness of the situation, such reflections may also signify a robust reflective capacity – this hypothesis is to be evaluated in future studies.
The feedback from the next group of 4 mother-infant dyad of participants who completed ACCESS BEAR in its entirety, was largely positive. Program acceptability was high with excellent retention rates. Three of the four dyads (75%) had a 100% attendance rate, and only one dyad missed one session. The mere availability of the program was appreciated as a priority with technical difficulties and saturation of screen time as common themes. The program components targeting emotional interaction and affect co-regulation were remarked and reflected upon, for example, one mother reflected:
I think it was just getting used to the platform and the technology. But um yeah, I think it worked well. And I, I really appreciated the fact that um the facilitators were really clear about, you know, we didn’t need to mute ourselves if our babies were crying, or having, you know, big feelings, like, that was fine. And I think that was actually, really positive, because it’s kind of…yeah it helped with that um, you know, getting more comfortable with it as just being a different mechanism to communicating.
The rapid adaptation to ACCESS BEAR has also provided our group of clinicians with techniques needed to deliver the program including experience in successful engagement of families and infants, online. Some challenges regarding family assessments including safety, deterioration of mental health, including partners and infants, pertained to limitations associated with having the therapeutic frame limited by the screen as one clinician observed, “it was harder to see the dyad interaction due to the camera – you often only saw one side of the interaction”. Establishing a plan for each family set the tone about managing issues and participating in this new mode of delivery.
In terms of the content delivery, the clinicians also remarked on the challenge of working with high levels of distress in the context of video technology:
There was one session about week 3 where a baby cried for the best part of a full hour. We paused the session…it was important for us to stop when babies have big feelings… It was hard for the families to hear, and we did acknowledge that it is hard, but we do need to hear babies even when their feelings are big. It was challenging to be with as a clinician in the face-to-face sessions we would have helped the mother take a break and help the infant to organise themselves with the mother. It felt a little like we intruded on this mother and infant in a most challenging time for both… we did speak to that mother after the session – it was too hard for her to hear us so she moved away from the camera, although we could hear her infant protesting. It was such a brave mother who allowed us to see her baby struggling – for the other mothers and infants, this moment helped explore that infants are participants in the group and that we need to allow space at times for this.
In terms of infant interaction with the program, the clinicians wondered if the infants were generally more settled at home, due to surprisingly notably fewer episodes of distress and disorganisation. Whilst the babies seemed delighted in the welcoming song each week, their engagement with other babies and the facilitators was reportedly more difficult to gauge. Infant responsiveness and engagement of the mother and of the program, raise important research and clinical considerations. For example, with regards to the objective evaluation of infant mental state, when the infant is at a distance, and when the visibility of the interaction is limited by video.
Both participant and clinician feedback suggest online delivery of ACCESS BEAR is potentially a promising enterprise. It would provide a valuable addition to face-to-face BEAR programs in allowing engagement with difficult to reach and remote populations. However, the differences in the modes of delivery regarding virtual and videoconference use for ACCESS BEAR, including program effectiveness, remain to be evaluated in future studies in terms of infant outcomes, mental health, and the quality of the parent-infant interaction.
Clinical Implications
The above discussed perspectives highlight the importance of the availability of ongoing support and clinical intervention, with regards to challenges associated with emotional aspects of early parenting, for at-risk families during COVID-19. However, the consideration of the assessment of mental state and safety remains of significant importance. The continuation of face-to-face service delivery for most vulnerable families is therefore preferable.
In terms of assessment of infant engagement with online programs, coding principles of attachment-based measures and atypical parental behaviours (e.g., (Tronick & Chon 1989; Lyons-Ruth, Bronfman, & Parsons 1999; Lyons-Ruth & Spielman 2004) are required to be translated from research to practice with more urgency in the context of the current global pandemic.
Screening measures such as the Edinburgh Post Natal Depression Scale (Cox et al., 1997) and the Mother Infant Relationship Scale (Newman-Morris et al., 2020) should be made widely accessible in online formats for the prompt screening of maternal mood, and relationship quality, and used to inform specific engagement with services, and modes of treatment delivery.
Further, the use of video-feedback approaches as methods of intervention, and assessment, or observation, require further research and evaluation in the context of a broader move to the use of online parent-infant psychotherapy service delivery.
Importantly, the integration of screening and relational assessments with online therapeutic interventions allows for monitoring of the longer-term developmental impacts of the pandemic on attachment and infant developmental outcomes.
Conclusion
The established Building Early Attachment and Resilience program (BEAR; Newman, 2012, 2015) was rapidly adapted for distance delivery mode via video technologies (ACCESS BEAR) in response to the urgent clinical need to support parents and infants following the withdrawal of community group programs and home visiting. The ACCESS BEAR program has been piloted and delivered to 9 dyads. Overall, both participant and clinician feedback has been positive with value placed on social connectedness, learning about infant development and interaction, and access to clinical support. This suggests infant mental health programs developed for vulnerable groups may be well received in online formats. However, empirical research is urgently required to evaluate the effectiveness of the program in terms of infant outcomes, maternal mental health, issues related to assessment and evaluation of mental state, and risk via remote technologies, as well as economic service delivery evaluations. Longitudinal intervention studies evaluating the effectiveness of BEAR programs, including ACCESS BEAR, are underway. More research is required regarding virtual and online delivery of parent-infant programs, including critical discussions and evaluation of the impact of a potential cultural shift to online modes of delivery of psychotherapy more broadly.
References
Barisic, A. (2020). Conceived in the COVID-19 crisis: Impact of maternal stress and anxiety on fetal neurobehavioural development. Journal of Psychosomatic Obstetrics & Gynaecology,41, 246.
Berthelot, N., Lemieux, R., Gavon-Bisonnette, V., Drouin-Maziade, C., Martel, E., & Maziade, M. (2020). Uptrend in distress and psychiatric symptomatology in pregnant women during the COVID-19 pandemic, Acta Obstet Gynecol Scand, 848-855. 17 June online, https://doi.org/10.1111/aogs.13925
Brooks, S.K., Weston, D., Greenberg, N. (2020). Psychological impact of infectious disease outbreaks on pregnant women: rapid evidence reviews. medRxiv https://doi.org/10.1101/2020.04.16.20068031
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150, 782–786.
Farrell, T., Reagu, S., Mohan, S., Elmidany, R. (2020). The impact of the COVID-19 pandemic on the perinatal mental health of women. Journal of Perinatal Medicine, 25 September online, https://doi.org/10.1515/jpm-2020-0415
Granqvist, P., Sroufe, L. A., Dozier, Hesse, E., Steele, M., Van IJzendoorn, M., . . . Duschinsky, R. (2017). Disorganized attachment in infancy: A review of the phenomenon and its implications for clinicians and policy-makers. Attachment & Human Development, 19(6), 534-558.
Lyons-Ruth, K., Bronfman, E., & Parsons, E. (1999). Maternal frightened, frightening, or atypical behaviour and disorganised infant attachment patterns. In J. Vondra & D. Barnett (Eds.), Atypical attachment in infancy and early childhood among children at developmental risk. Monographs of the Society for Research in Child Development, 64 (3), 67-96.
Lyons-Ruth, K., & Spielman, E. (2004). Disorganised infant attachment strategies and helpless-fearful profiles in parenting: integrating attachment research with clinical intervention. Infant Mental Health Journal, 25(4), 315-335.
Main, M. (2000). The organized categories of infant, child, and adult attachment: Flexible vs. inflexible attention under attachment-related stress. Journal of the American Psychoanalytic Association, 48, 1055 – 1096.
Madigan, S., Cyr, C., Eirich, R., Pasco Fearon, R., Ly, A., Rash, C., . . . Alink, L. (2019). Testing the cycle of maltreatment hypothesis: Meta-analytic evidence of the intergenerational transmission of child maltreatment. Development and Psychopathology, 31(1), 23-51.
Marshal. J., Kihlstorm, L., Buro, A., Chandran, V., Prieto, C., Stein-Elger, R. et al., (2020). Statewide implementation of virtual perinatal home visiting during Covid-19. Maternal and Child Health Journal, online. https://doi.org/10.1007/s10995-020-02982
Newman L. K. (2012, 2015, 2019). Building Early Attachment and Resilience (BEAR)- an Attachment and Mentalisation Focused Intervention for Early Parenting – Facilitator Guide. Melbourne University: Melbourne, Australia.
Newman, L. K. (2015). Parents with borderline personality disorder. Australasian Psychiatry, 23(6), 696–698.
Newman, L., Sivaratnam, C., & Komiti, A. (2015). Attachment and early brain development – neuroprotective interventions in infant–caregiver therapy. Translational Developmental Psychiatry, 3(1): 28647.
Newman-Morris, V. Gray, K., Simpson, K., Newman, L. K. (2020). Development and Initial Reliability and Validity of a New Measure of Distorted Maternal Representations: The Mother-Infant Relationship Scale. Infant Mental Health Journal, 41, 40–55. https://doi.org/10.1002/imhj.21826
Nugent, J. K., Keefer, C. H., Minear, S., Johnson, L. C., & Blanchard, Y. (2007). The newborn behavioral observations (NBO) system handbook. Baltimore, MD, US: Paul H Brookes Publishing.
Oates, J. (2007). Quality of Care for Young Children: Attachment Relationships. The Open University, Milton Keynes.
PANDA (2020). The coronovirus pandemic has seen calls for help from new parents skyrocketing. https://www.panda.org.au/news-media/the-coronavirus-pandemic-has-seen-calls-for-help-from-new-parents-skyrocketing
Preis, H., Mahaffey, B., Heiselman, C., Lobel, M. (2020). Pandemic-related pregnancy stress and anxiety among women pregnant during the COVID-19 pandemic. The American Journal of Obstetrics & Gynecology Maternal-Fetal Medicine 2, 100155. https://doi.org/10.1016/j.ajogmf.2020.100155
Russo, S. J., Murrough, J.W., Han, M., Charney, D. S., & Nestler, E. J. (2012). Neurobiology of resilience. Nature Neuroscience, 15, 1475-84.
Schore, A.N. (2010). Relational trauma and the development of the right brain: The neurobiology of broken attachment bonds. In: Barandon T, editor. Relational trauma in infancy: Psychoanalytic, Attachment and Neuropsychological Contributions to Parent infant Psychotherapy. London: Routledge, 2010, 19-48.
Slade, A., Holland, M., Ordway, M., Carlson, E., Jeon, S., Close, N., . . . Sadler, L. (2020). Minding the Baby®: Enhancing parental reflective functioning and infant attachment in an attachment-based, interdisciplinary home visiting program. Development and Psychopathology, 32(1), 123-137. https://doi:10.1017/S0954579418001463
Tronick, E., & Cohn, J. (1989). Infant-mother face-to-face interaction: Age and gender differences in coordination and miscoordination. Child Development, 59, 85-92.
Thapa, S. B., Maiali, A., Scwab, S., & Acharya, G. (2020). Maternal mental health in the time of the COVID-19 pandemic, Acta Obstetricia et Gynecologica Scandnivica, 99, 817-818.
Authors declare no conflict of interest.
Correspondence:
Angela Komiti
Postal Address:
Department of Psychiatry
Level 1 North,
Main Block, Royal Melbourne Hospital,
Parkville VIC 3050
Australia
Email: angelaak@unimelb.edu.au
Authors
Newman, Louise, PhD
Department of Psychiatry, Faculty of Medicine, Dentistry and Health Sciences
The University of Melbourne, Parkville, Victoria 3052, Australia
Newman-Morris, Vesna, PhD
Department of Psychiatry, Faculty of Medicine, Dentistry and Health Sciences
The University of Melbourne, Parkville, Victoria 3052, Australia
Komiti, Angela, PhD
Department of Psychiatry, Faculty of Medicine, Dentistry and Health Sciences
The University of Melbourne, Parkville, Victoria 3052, Australia
Gammell, Beth,
Department of Psychiatry, Faculty of Medicine, Dentistry and Health Sciences
The University of Melbourne, Parkville, Victoria 3052, Australia
Braden, Alice, MPsych
Department of Psychiatry, Faculty of Medicine, Dentistry and Health Sciences
The University of Melbourne, Parkville, Victoria 3052, Australia
Carron, Sarah-Pia, DPsych
Department of Psychiatry, Faculty of Medicine, Dentistry and Health Sciences
The University of Melbourne, Parkville, Victoria 3052, Australia