Abstract
The Australian Government’s policies and action plans referencing infant mental health have coincided with calls from infant mental health professionals seeking greater support within the infant mental health sector. Broadly, infant mental health refers to an individual’s ability to respond physically and emotionally to their surrounding environment, encompassing regulative behaviours and social and cognitive abilities. This paper considers the impact of optimising parent-infant relationships on the applicability of public health science when implemented within a community-based setting by exploring a proof-of-concept, innovative practice model in promoting infant mental health. This novel infant mental health promotion program was delivered as a weekly intervention over ten weeks. It was conceptualised using public health science to promote infant and maternal mental health. The program sought to capitalise on existing infant-parent interaction activities embedded within community activities, which for this case study included a baby learn to swim class.
Introduction
Increasing recognition of the influential role of the parent-infant relationship, and infant mental health needs more broadly, represents a landmark for opportunities to advance infant mental health promotion (NMHC, 2019; 2021; NSCDC, 2020; Priddis et al., 2018; Schore, 2001; UK Gov, 2018). The parent-infant relationship has long been recognised as fundamental to enhancing infant mental health (Fraiberg, 1980). Everyday parent-infant interactions support the development of the attachment relationship, forming foundations for lifelong mental health (NSCDC, 2020; Schore, 2001; Zeanah, 2019). Following recommendations from recent Australian frameworks such as the ‘National Children’s Mental Health and Wellbeing Strategy’ and the ‘Brighter Beginnings: First 2000 Days of Life’ strategy, it is important to explore how infant and maternal mental health can be supported within the community.
This paper describes an innovative practice model for promoting infant mental health and optimising parent-infant relationships in the first year of life. The case study explores the applicability of public health science at a foundational level when informed by community-health and community-centred frameworks. This proof-of-concept study was designed to examine the feasibility and acceptability of a psychoeducational program implemented in conjunction with a parent-baby swim class.
Background
The early emotional interactions between infants and their primary caregivers, and the attachment relationship they form, shape infants’ neurological and psychosocial development in ways that influence their developing capacity for stress adaptation and resilience (Newman et al., 2016). A comprehensive body of evidence indicates that disruptions in these early caregiving relationships are associated with reduced positive short and long-term outcomes for the infant (Stolper et al, 2021; Newman et al., 2016; Stein et al., 2014).
The inaugural Australian National Children’s Mental Health Strategy (NMHC, 2021), launched in September 2021, is focused on promoting the mental health and wellbeing of children beginning in the perinatal period, and supporting all children in their communities to thrive. The strategy’s brief is to establish an Australian context that supports the shared role of families, communities, services, and educators in nurturing, promoting, and supporting child mental health. This landmark strategy represents an attempt to actively promote child mental health and wellbeing using child-centred, universal, and targeted approaches, situated within a climate of burgeoning and multidisciplinary interest in early life relationships, parent-infant interactions, and experiences for positive developmental trajectories.
The strategy articulates the importance of promoting quality early life relationships to optimise developmental trajectories using the relational framework approach of infant mental health and the ‘science of experience’ (NMHC, 2021; Zeanah & Zeanah, 2019). A relational framework acknowledges that parent-infant interactions provide the context for infants’ growth and development and the foundations for developing a secure infant attachment relationship (Newman et al., 2016; NSCDC, 2020).
Much of the multidisciplinary work of infant mental health has taken place within a healthcare services framework. Ten years ago, results of the first comprehensive, nationwide longitudinal study of Australian children’s mental health prompted calls for a public health perspective beginning in infancy. Simultaneously, in the public health space, Nelson and Mann (2011) and Miles et al. (2010) outlined the importance and benefits for social and emotional wellbeing, of enhancing early relationships.
The application of public health science within the field of infant mental health can grow the availability and accessibility of infant mental health promoting initiatives and settings. Providing communities with opportunities and support for promoting infant social-emotional wellness can create conditions favourable for optimising infant mental health (NMHC, 2021, Miles et al., 2010, Nelson & Mann, 2011). Nelson and Mann (2011) endorsed this concept by supporting approaches that capitalise on the daily responsive interactions between children and their primary caregivers. Communities centred around daily interactions between an infant and their caregiver represent an ideal location for building, embedding, and promoting infant mental health. Furthermore, as recently as 2020, the Executive Director of the National Mental Health Commission acknowledged the role of communities in the experience of mental health and wellbeing and the importance of the system responding at this level.
Despite the continued growth in support for this model of care, practical implications require embedding practices within the communities where infants and their families live. Community-based parent-infant activities provide a valuable platform offering parents and caregivers education and support in the importance of providing nurturing, responsive environments, fostering relationships, and promoting mental wellness (Nelson & Mann, 2011; NRCIM, 2000; Zeanah et al., 2005; NMHC, 2021; NSW Gov., 2019).
The ‘National Children’s Mental Health and Wellbeing Strategy’ (NMHC, 2021) first focus area is Family and Community. This area emphasises community-based approaches as fundamental in empowering families to promote the mental health and wellbeing of their children through everyday parenting. Similarly, the NSW Government’s ‘Brighter Beginnings: First 2000 Days of Life’ strategic framework (NSW Gov., 2019) focusses on supporting all children in NSW to have the best start in life through building a better understanding of the lifelong importance of the first 2000 days of a child’s life, connecting services and supports and providing easy access to timely information and services. These overarching strategy commitments highlight the importance of community-based activities.
Both the community-health and community-centred promotional and preventative models incorporate public-health science through the involvement of supports outside of the healthcare system to deliver information and services in trusted environments without the involvement of medical or pharmaceutical therapy (Heath, 2020; UK Gov., 2018). This delivery model engages skilled community members, local groups, networks, and physical, environmental, and economic resources to promote, encourage and influence health-related behaviours (UK Gov., 2018). A review of this model of support has revealed robust, meaningful results at the population level when delivered within the context of public health education, social marketing, health promotion and policy change in recognition of the multiple determinants of health (IOM, 2012).
A case study of a community-embedded infant mental health initiative
In Australia, parent-baby swim classes are often well-known and attended activities within communities involving both parents and their babies. Parent-baby swim classes have traditionally aimed to provide babies with water familiarisation opportunities, to build baby’s comfort, interest and confidence in the water and develop simple water safety skills. It is not uncommon for some babies to experience difficulties with settling in the ‘class’ and well-intended, uninformed, and unhelpful socio-cultural explanations and tactics may be applied to an unsettled infant in swim class. Socio-cultural expectations may contribute to a parents’ felt experience of ‘inadequacy’ or ‘judgement’ from peers when their baby is not settled in the class and there are low levels of awareness/confidence of the skills and abilities for settling a baby in a social environment. Swim teachers of babies do not currently receive training in parent-infant mental health, although they are working directly with parent-infant dyads.
The program ‘Mums and Bubs Get Wet for Wellbeing’ was conceptualised from these observations and from an understanding that infants’ everyday experiences, moment to moment, in their world are continuously contributing to their meaning-making about themselves in relation to their world (Tronick & Beeghly, 2011), in turn, shaping their ongoing engagement with the world. The infant-parent dyad represents a mutually regulated system of communication continuously operating to provide scaffolding of the infants’ engagement with the world around them (Tronick & Beeghly, 2011). The potential for these weekly 30 minutes sessions to be truly dyadic in nature and capitalise on the availability of skin-to-skin contact in a warm soothing body of water, face to face interaction, as well as play and exploration, was realised; Mums and Bubs Get Wet for Wellbeing was ‘born’.
The aims of the program were to support and improve, 1) maternal psychosocial wellbeing, 2) sensitive and responsive parenting skills, 3) mother-infant connection and bonding, and 4) infant social-emotional development experiences. The proof-of-concept design with a focus on feasibility and acceptability would allow our intervention to serve as a new model for developing community-embedded mental health initiatives reflecting an infant mental health promotion initiative addressing the action areas of the Ottawa Charter for Health Promotion (WHO, 1986). For example, by creating supportive environments, strengthening community action, developing personal skills, reorienting health services, and aligning with overarching current healthy public policies.
Method
Setting
The pool where (Mums and Bubs Get Wet for Wellbeing) the program was implemented is a recognised community gathering place (pool and centre) for individuals and families of all ages and backgrounds. The program was implemented in the Lake Macquarie region of New South Wales, Australia, with around 200,000 people, including >32,000 families with children. The pool centre has an established community swim school, located within Toronto’s ‘First Splashes’ swim centre, offering Learn to Swim programmes and Aquatics Survival Skills to ~12,000 parent-baby dyads annually. All swimming instructors are AUSTSWIM accredited, the Australian industry standard for Swimming and Water Safety Teachers™.
The strong and positive presence of the pool and centre within this community of Aboriginal (4.45%) and non-Aboriginal and peoples and people born overseas (3.34%) (LMCC, 2022) provided an ideal setting to deliver a family and community mental health and wellbeing initiative, as emphasised in the National Children’s Mental Health and Wellbeing Strategy (NMHC, 2021). Parent-infant swim classes are well attended (~12,000 parent-baby dyads annually) in this highly regard family-friendly community setting. This initiative, capitalised on this established parent-infant activity in the community to embed an infant mental health promotion initiative that aligns with current healthy public policy including addressing programme/services accessibility; a known common barrier to treatment and social determinants of health (Pearn et al., 2020, NMHC, 2021).
The embedding of infant mental health promotion initiatives within existing community-based parent-infant activities represents an incredible potential for wide-reaching accessibility/availability of infant mental health promotion action. One such community-based activity is parent-infant swim classes, with an estimated 4.2 million Australian children participating in swimming lessons each year. Incorporating a focus on both the child and the parent is a key component in the ‘National Children’s Mental Health and Wellbeing Strategy’s’ (2021) objectives of supporting families, increasing mental health literacy through community-driven approaches.
Recruitment
Over four months, recruitment invitations were shared via local mental health services (private, public, NGO), GP surgeries, mothers’ groups, and the Toronto Swim Centre. Inclusion criteria were mothers and babies (aged between 4-12 months) from the Lake Macquarie region of New South Wales, Australia. The inclusion criteria were broad to increase accessibility as per a universal public health perspective.
Participants
Twenty-three mothers expressed interest in the program, with fourteen participants enrolling. The infant age range was 4 to 11 months; 11 babies were female, one baby was from a culturally and linguistically diverse background, and one was of Aboriginal and Torres Strait Islander background. Most had found out about the program from friends or their mothers’ group or the swim centre. One participant withdrew after week one. Thirteen participants completed the program. Out of these 13 participants, 12 completed pre-program questionnaires, but only eight completed post-program questionnaires. All 13 participants indicated a willingness to be interviewed when providing consent, with eight participants completing interviews at the conclusion of the program.
Program
The community-embedded program ‘Mums and Bubs Get Wet for Wellbeing’, designed by the authors DC, RE, LC, and VM, targeted 1) maternal psychosocial wellbeing, 2) sensitive and responsive parenting skills, 3) mother-infant connection and bonding and 4) supported infant social-emotional development experiences in each phase of the study through psychoeducation sessions, attachment-focused swimming classes and peer support seen within a three-phase approach.
Phase one
Nine AUSTSWIM instructors completed two days of training based on attachment theory, perinatal mental health, and infant development to enhance knowledge of healthy mother-infant interactions during swimming sessions. Teachers were taught to coach and support mothers to notice, observe, and attune to their baby’s needs.
Phase two
The mother-baby dyads participated in ten weekly 30-minute swimming lessons facilitated by a program-trained swimming instructor. Two groups including seven dyads, were offered. The program was delivered free of charge with classes focusing on mother-baby interactions (including activities encouraging face-to-face, skin-to-skin, and touch) and uninterrupted time for babies to experience mutual play, communication, and reciprocity. An accredited mental health social worker (VM) joined the teachers in the pool and supported the swim session by observing the dyads and reflecting on infant behaviours to lead mothers in exploring, interpreting, and appropriately responding to behaviours displayed by their children. The support worker used questions such as “Do you think they enjoyed that? “Why/why not?”, “How do you know?” to highlight non-verbal communication used by the infants to encourage deeper interaction and subsequent bonding.
Phase three
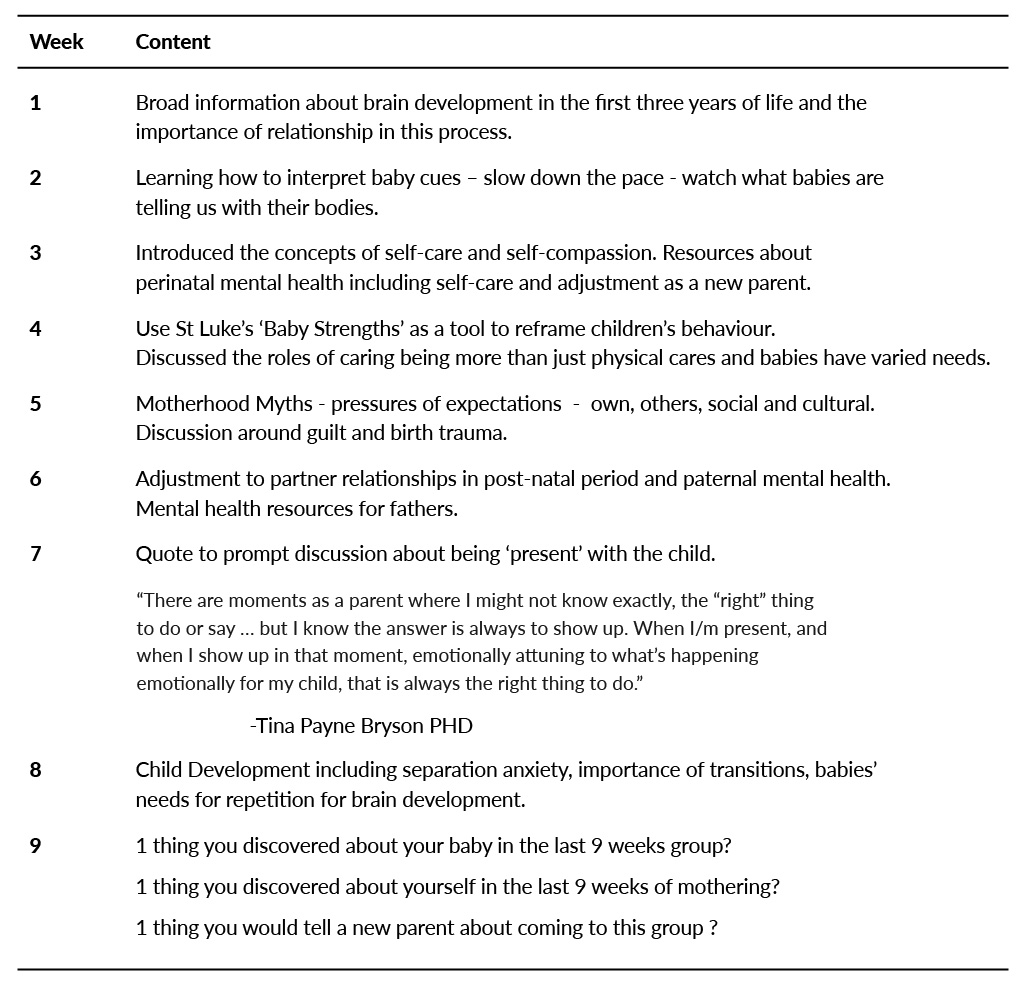
Mothers and their babies were invited to attend a tea and coffee catch-up education session following each water-based session. Sessions ran for ~45 minutes and were facilitated by a mental health social worker (VM). The session began with a semi-formal, 20-minute presentation on maternal mental health and wellbeing topics, including postnatal depression (see Table 1). Subsequently, participants were encouraged to engage in unstructured social discussions with the other mothers.
Table 1. Topics for Mums and Bubs Tea & coffee catch-up.
Program evaluation
To undertake the proof-of-concept evaluation, a three-step mixed methods design was used. The evaluation process was approved by the Human Ethics Committee at the University of Newcastle (H-2021-0136).
1) Feasibility was assessed by collecting data on recruitment and retention rates (number of participants who accessed and completed the program), adherence rates, recruitment (time required to recruit), the feasibility of testing procedures, and data collection methods including completion rates.
2) Following informed consenting procedures, mothers were asked to complete a survey before and end of the program:
-
- The pre-program survey contained questions related to participant demographics and parent experiences of psychological distress; and
- At the end of the program, the participants completed a measure of psychological distress and an evaluation form. The 21-item Depression Anxiety Stress Scale (DASS-21; Lovibond & Lovibond, 1995) included a standardised and well-validated tool to measure psychological distress.
3) After completing the program, consenting participants completed semi-structured individual interviews, consisting of open questions about the pre-planned research questions relating to feasibility and acceptability, including maternal psychosocial wellbeing, sensitive and responsive parenting skills, mother-infant connection, and bonding, and supported infant social-emotional development experiences.
The questions were designed to elicit information leading to practical recommendations and evaluations of the program. Individual interviews were determined to be the most appropriate data collection method due to the richness of data available from first-hand accounts of participant experience (Poole et al., 2012).
The questions explored participants’ expectations, experiences, satisfaction, and feedback, with follow-up questions and prompted for clarification and elaboration as appropriate. Interviews were completed by the author R.S via the teleconferencing tool, Zoom for Education. The video function was optional. Interviews were password-protected to ensure security. Verbatim interview transcripts were obtained, with a preliminary transcript provided by Zoom software and manual audio file cross-referencing. The average duration of each interview was 15 minutes.
Data Analyses
Primary feasibility data, including recruitment, retention rates, adherence rates, and survey data, were analysed using the statistical software JASP (version 0.14.1) with simple frequencies and descriptive analysis exploring the pre-and post-test survey data.
Transcripts were imported into NVivo (version 12) for coding and thematic analysis by RS to explore acceptability. Thematic analysis was chosen as it is a transparent and systematic approach to identifying shared themes. The analysis was conducted within a realist/essentialist paradigm (Boyatzis, 1998). It included identifying, analysing, and reporting patterns identified within interviews, where patterns indicated reoccurring concepts as potential themes (Braun & Clarke, 2006). Inductive and deductive thematic analysis was used (Guest et al., 2012).
Familiarity with the scripts was attained by the repeated active reading of each transcript, revealing preliminary themes. An iterative process of refining the themes was carried out by reviewing the data set, ensuring internal and external representativeness (Braun & Clarke, 2006). A re-reading of the scripts was carried out to ensure the validity of the data by establishing that the themes accurately represented the data set. The process and themes were reviewed and agreed upon by the other authors. Evidentiary quotes taken from participant interviews support the themes. Deidentified quotes are presented verbatim.
Results
Survey results
Eight of the 12 participants who completed the pre-program questionnaires scored in the ‘normal’ range on each DASS-21 subscale in the pre-program questionnaires. Three women scored in the mild-moderate range for depression and anxiety, and three scored in the mild-severe range for stress. Of the eight participants who completed the post-program DASS-21, 5 had ‘normal’ scores across the subscales. Two women scored in the mild-moderate range for depression, and three scored in the mild-moderate range for stress.
Interview results
All 13 participants indicated a willingness to be interviewed when providing consent, with eight participants completing interviews at the conclusion of the program.
The views and experiences of the participants are collated in Table 2, with the thematic findings presented under a series of headings with illustrative quotes. Briefly, the themes included Attachment, Engagement, Educators, Learning and Relationships. All the participants reported positive experiences with opportunities to bond with their children through supportive playful activities, although a few women indicated that it was at times a bit anxiety-provoking to be observed. All women found the information provided was useful and relevant and all women enjoyed the opportunity to share experiences and connect with other new mothers. A few women suggested that it is important to consider the timing and structure of the classes to reduce barriers to participation e.g., considering nap times and it was also proposed by a few women to make similar training available to caregivers regardless of gender.
Table 2. Themes for Qualitative Thematic Analysis to Evaluate Participant Views and Experience.

Discussion
The current paper describes an innovative community-embedded infant mental health promotion practice model as a case study for a public health promotion initiative that meets the Ottawa Charter’s (WHO, 1986) action areas of strengthening community action, developing personal skills, creating supportive environments, reorienting health services within a context of new healthy public policy (NMHC, 2021) for infant mental health. This infant mental health promotion initiative presents an example of policy translation in a context-specific way (Foley, 2021).
The initiative operationalises both the ‘National Children’s Mental Health and Wellbeing Strategy’s’ (NMHC, 2021) Family and Community focus area objectives (supporting families, increasing mental health literacy and community drive approaches) and the NSW Government’s ‘Brighter Beginnings: First 2000 Days of Life (best start in life by providing parents access to universal and targeted information) within an existing, highly regarded community-based parent-infant interaction activity.
The program was designed to be an experiential infant mental health promotion initiative, conceptualised using public health science to promote infant and maternal mental health. The program’s centrality on the relational framework approach (Priddis et al., 2018; Zeanah, 2019) engages the infant-parent interactions taking place within existing community activities, in this model, baby learn to swim classes. The evaluation provided proof-of-concept for this type of program with data supporting reasonable recruitment and retention throughout the program, high acceptability from the participating mothers but with some problems collating survey-based information (only 8 out of 13 completing the post-program survey).
Embedding psychoeducational programs in local settings and services that parents are naturally inclined to seek out presents an opportunity to provide universal access to mental health promotion. The NSW Government’s ‘Brighter Beginnings: First 2000 days of Life’, aims to give children the best start in life through providing parents and families with universal and targeted access to the right information and at the right time (NSW Gov., 2019). The National Children’s Mental Health Strategy (NMHC, 2021) establishes at a national policy level the importance of supporting families beginning in the perinatal period, identifying parents who may be struggling, promoting parenting at key developmental stages to support child development, increasing mental health literacy, and reducing stigma through whole communities, developing strong and supportive relationships within and outside children’s homes.
Mums and Bubs Get Wet for Wellbeing delivers on the Strategy’s (NMHC, 2021) priority action areas of:
- Routine offering of evidence-based parenting ‘programs’ at key developmental milestones, emotional wellbeing modules embedded in parenting courses;
- Widely accessible evidence-based resources building on existing initiatives; and
- Campaigning to promote the value of parenting.
A broad range of recruitment methods made it possible to recruit mothers to the groups, and the retention, and engagement, of participants in the program, were excellent with only one participant discontinuing the program (although not all chose to complete the surveys or participate in the interviews). The interviews revealed that while sickness or other unavoidable commitments inevitably affect attendance, it is also important to consider what time of the day the program is delivered, with nap times and commitments for other children being considered for participation.
The program design received positive feedback. The mothers mentioned how the playfulness of the program helped in their bonding experience with their children. Mothers indicated that being ‘compared’ to other mothers or ‘judged’ by professionals can be a worry. This highlights the need for swim teachers and facilitators to be mindful of such thoughts and provide skills to communicate effectively and empathically through normalising validating the mother’s experience.
While the structure of the sessions was generally positively reviewed, there was a desire to make the social get-togethers more organised with a specific end-time to make daily planning easier. It was also clear that mothers were seeking support, not only for themselves but for their partners, and this is an important consideration in future projects.
As with many other evaluation processes, it was difficult to obtain surveys and feedback (both via survey and interviews) from all participants to ensure the sample’s representativeness. While the excellent retention and engagement, with only one participant discontinuing, support the feasibility and acceptability of the program, to evaluate the effectiveness of infant and parental mental health, this hurdle needs careful planning to scale this proof-of-concept study up.
Community embedded initiatives present an opportunity to prevent stigma arising from selection into programs based on need or risk and support families not identified in targeted and selective mental health services. This provides an avenue for further exploration on how to implement such approaches not only in learning to swim classes but in other community embedded activities that parents in the perinatal period participate in such as, e.g., play and library groups. This would facilitate universal availability in line with recommendations on the positioning and effectiveness of promotion and prevention approaches in infant mental health (McLuckie, 2019; NHMRC, 2017).
Universally available programs of prevention and promotion approaches for maternal and infant mental health are uniquely placed to optimise healthy perinatal periods for infants, their parents, and caregivers, supporting what is needed to set up and advance the healthy development of the future generations of children and adults.
Clinical Implications
This type of program can fill identified gaps within the perinatal mental health field, which is overwhelmingly costly when not addressed, currently considerably under-resourced, yet highlighted in the policy and funding space (NRCIM, 2000). A focus on universally available group approaches incorporating community-health and community centred promotion and prevention approaches can strengthen maternal and infant mental health care, facilitating a widening availability of practices, activities, information, and resources into communities and providing increased options for mothers, their infants, and families, during the perinatal period.
This opportunity presents fortuitously within the presently aligned Australian (National Children’s Mental Health and Wellbeing Strategy, NMHC, 2021) and NSW (NSW Government’s Brighter Beginnings First 2000 days, NSW Gov, 2019) policy climate, focusing on increasing acceptability and accessibility of the beneficial opportunities and experiences for mothers, infants, and their families, during the critical period when foundations for future mental health are being constructed.
References
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
Boyatzis, C. J. (1998). A collaborative assignment on the role of culture in child development and education. Teaching of Psychology, 25(3), 195- 198. https://doi.org/10.1207/s15328023top2503_7
Foley, M. (2021). Perspectives in Infant Mental Health: Special issue call for papers Infant Mental Public Health Promotion and Policy: Prioritising infant mental health in public health. WAIMH Perspecectives in Infant Mental Health, 29 (2) 2021_2_Perspectives_IMH_29_10_2021_published.pdf (waimh.org)
Fraiberg, S. (1980). Clinical Studies in Infant Mental Health (S. Fraiberg, Fraiberg, Louis, Ed.). Basic Books.
Guest, G., MacQueen, K. M., & Namey, E. E. (2012). Introduction to applied thematic analysis. Applied Thematic Analysis, 3(20), 1–21. https://doi.org/10.4135/9781483384436.N1
Heath, S. (2020). Difference between community health, community-based health. Patient Engagement Hit Website. https://patientengagementhit.com/news/the-difference-between-community-health-community-based-health
IOM (2012). An integrated framework for assessing the value of community-based prevention. The National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK206926/
McLuckie, A., Landers, A. L., Curran, J. A., Cann, R., Carrese, D. H., Nolan, A., Corrigan, K. & Carrey, N. J. (2019). A scoping review of mental health prevention and intervention initiatives for infants and preschoolers at risk for socio-emotional difficulties. Systematic Reviews, 8(1), 183. https://doi.org/10.1186/s13643-019-1043-3
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. https://doi.org/10.1016/0005-7967(94)00075-U
Miles, J., Espiritu, R. C., Horen, N., Sebian, J. & Waetzig, E. (2010). A Public health approach to children’s mental health. Georgetown University Center for Child and Human Development, National Technical Assistance for Children’s Mental Health. https://gucchd.georgetown.edu/products/PublicHealthApproach.pdf
Nelson, F., & Mann, T. (2011). Opportunities in public policy to support infant and early childhood mental health: The role of psychologists and policymakers. American Psychologist, 66(2), 129. https://doi.org/10.1037/A0021314
Newman, L., Judd, F., Olsson, C. A., Castle, D., Bousman, C., Sheehan, P., Pantelis, C., Craig, J. M., Komiti, A., & Everall, I. (2016). Early origins of mental disorder – risk factors in the perinatal and infant period. BMC Psychiatry, 16, 270-270. https://doi.org/10.1186/s12888-016-0982-7
NRCIM (2000). From neurons to neighborhoods: The science of early childhood development. (J. P. Shonkoff & D. A. Phillips, Eds.). Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK225562/
NHMRC (2017). Promoting social and emotional development and wellbeing of infants in pregnancy and the first year of life. National Health and Medical Research Council. https://www.nhmrc.gov.au/about-us/publications/promoting-social-and-emotional-development-and-wellbeing-infants-pregnancy-and-first-year-life
NHMC (2020). Mental Health Reform. Australian Government. https://www.mentalhealthcommission.gov.au/Mental-health-Reform
NHMC (2021). National Children’s Mental Health and Wellbeing Strategy. Australian Government. https://www.mentalhealthcommission.gov.au/getmedia/5b7112be-6402-4b23-919d-8fb9b6027506/National-Children%E2%80%99s-Mental-Health-and-Wellbeing-Strategy-%E2%80%93-Report
NSCDC (2020). Connecting the brain to the rest of the body: early childhood development and lifelong health are deeply intertwined. Harvard University. https://developingchild.harvard.edu/resources/connecting-the-brain-to-the-rest-of-the-body-early-childhood-development-and-lifelong-health-are-deeply-intertwined/
World Health Organisation. (1986). Ottawa Charter for Health Promotion: First International Conference on Health Promotion Ottawa, 21 November 1986. https://www.healthpromotion.org.au/images/ottawa_charter_hp.pdf
Pearn, J., Peden, A., & Franklin, R. (2020). Drowning of pet owners during attempted animal rescues: The AVIR-A syndrome. International Journal of Aquatic Research and Education, 12(2). https://doi.org/10.25035/ijare.12.02.08
Poole, R., Simpson, S. A., & Smith, D. J. (2012). Internet-based psychoeducation for bipolar disorder: a qualitative analysis of feasibility, acceptability, and impact. BMC Psychiatry, 12(1), 139–139. https://doi.org/10.1186/1471-244X-12-139
Priddis, L. E., Matacz, R. A., Kiely, D., Bayes, S., Barratt-Pugh, C., Pooley, J. A., Lauren, C., Thornton, J., Fitzgerald, H. E. (2018). Better Together: Supporting Perinatal and Infant Mental Health Services. WA Primary Health Alliance and Edith Cowan University. https://bcec.edu.au/assets/2019/08/Better-Together-Supporting-Perinatal-and-Infant-Mental-Health-Services-BCEC-Report-2019.pdf
Schore, A. N. (2001). Effects of a secure attachment relationship on right brain development, affect regulation, and infant mental health. Infant Mental Health Journal, 22(1-2), 7-66. https://doi.org/https://doi.org/10.1002/1097-0355(200101/04)22:1<7::AID-IMHJ2>3.0.CO;2-N
Stein, A., Pearson, R. M., Goodman, S. H., Rapa, E., Rahman, A., McCallum, M., Howard, L. M., & Pariante, C. M. (2014). Effects of perinatal mental disorders on the fetus and child. The Lancet, 384(9956), 1800-1819. https://doi.org/https://doi.org/10.1016/S0140-6736(14)61277-0
Stolper, H., van Doesum, K., & Steketee, M. (2021). How to Support Parents of Infants and Young Children in Mental Health Care: A Narrative Review [Review]. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.745800
Tronick, E., & Beeghly, M. (2011). Infants’ meaning-making and the development of mental health problems. The American psychologist, 66(2), 107–119. https://doi.org/10.1037/a0021631
UK Gov. (2018). Health matters: community-centred approaches for health and wellbeing. https://www.gov.uk/government/publications/health-matters-health-and-wellbeing-community-centred-approaches/health-matters-community-centred-approaches-for-health-and-wellbeing
Zeanah, C. H., Jr. & Zeanah, P. D. (2019) Infant Mental Health, The Clinical Science of Early Experience. In C. H. Zeanah (Ed.), Handbook of Infant Mental Health. Guilford Press, NY.
Zeanah, P., Nagle, G., Stafford, B., Rice, T., & Farrer, J. (2005). Addressing Socio-Emotional Development and Infant Mental Health in Early Childhood Systems: Executive Summary. Building State Early Childhood Comprehensive Systems Series, Number 12. UCLA Center for Healthier Children, Families and Communities.
Authors
Campbell, Linda E.,
School of Psychological Sciences, University of Newcastle, Australia
Healthy Minds, Hunter Medical Research Institute, Australia
Costa, Deborah,
School of Psychological Sciences, University of Newcastle, Australia
Stacey, Rebecca K.,
School of Psychological Sciences, University of Newcastle, Australia
Mansfield, Vicki,
The Hummingbird Centre, Newcastle, Australia
Elliott, Rickie,
The Hummingbird Centre, Newcastle, Australia
Contact details:
Linda Campbell, School of Psychological Sciences, University of Newcastle, University Drive, 2308 Newcastle, Australia. Email: linda.e.campbell@newcastle.edu.au








