Policy Context
Programmes for Government in Scotland have consistently prioritised the lives of children, and in recent years have specifically focussed on the needs of babies and young children. The Perinatal and Infant Mental Health Programme Board (PIMH-PB) was set up in 2019 by the Scottish Government (SG), and its tasks include:
Creat(ing) a Scotland wide multiagency model of infant mental health provision to meet the needs of families experiencing significant adversity, including infant developmental difficulties, parental mental illness, parental substance misuse, domestic abuse and trauma. (SG, 2019a)
The mental health needs of infants from conception to three years of age are informing the development of systems that will support families where parents may not have access to formal mental health services. These systems include both statutory (health and local authority) and third sector services, and infants, parents and carers in service design and delivery. Third sector services offer a range of support, from volunteers offering practical support to families, peer support and befriending, through to specialist infant-parent work. McFadyen (2021) gives a detailed account of this work.
Public policy in Scotland is grounded in an understanding of the impact of inequality and disadvantage on early child development, and this informs both systems and practice in universal services. Maternity and health visiting pathways have been designed to support children and families through prevention, early identification, and intervention. Getting it Right for Every Child (GIRFEC) (SG, 2019b) provides a systemic approach to support parents, carers, statutory and voluntary agencies to work together to ensure the best outcome for every child. Routine inquiry enables maternity and health visiting services to gather sensitive data about the family circumstances of each infant and record the progress of each child’s development.
This Scottish framework for working together with the child at the centre is complemented by The Promise Scotland (2020) which aims “to ensure that every child grows up loved, safe and respected, able to realise their full potential”. The voice of the child (infant) is one of the 5 pillars of The Promise, and a key component of the UNCRC (Incorporation) (Scotland) Bill that was passed by the Scottish Parliament in 2021. The Fairer Scotland Duty (SG, 2018) places a legal responsibility on named public bodies to actively consider how they can reduce inequalities of outcome caused by socio-economic disadvantage.
The Social Determinants of Health
The relationship between health and poverty is bidirectional. Investing in early childhood development can boost shared prosperity, promote inclusive economic growth, expand equitable opportunity, and end extreme poverty (WHO, 2018). Children who experience poverty and other structural inequalities are more likely to experience adversities in their lives (Treanor, 2020; Shonkoff et al., 2021). Poverty and inequality can create conditions that undermine healthy pregnancy, healthy early relationships, effective support for caregivers, and a safe and stimulating early environment. Adversity in childhood is highly correlated with socioeconomic disadvantage in the first year of life (Marryat & Frank, 2019).
A study using Growing Up in Scotland (GUS) data, found that 11% of children in the lowest income quintile at birth had experienced 4+ adverse experiences by the age of 8, compared to 3% of children overall. At ages 3 and 5 years, there was a strong relationship between socio-economic inequality and gaps in children’s cognitive, emotional, and social development. Children whose mothers were emotionally well during their first four years had better social, emotional, and behavioural development than those whose mothers had brief or repeated mental health problems.
Marryat and Frank’s study focused on socio-demographic risks; they suggested that future research “may wish to explore the explanatory power of factors such as attachment, neurodevelopmental disorders, parenting and parental ACEs”. Tomlinson (2015) calls for research into “upstream” influences (such as socioeconomic status, discrimination, and political inequality) on infant mental health in order to “build the foundations for sustainable, equitable, and prosperous societies.”
Most recently, poorer infants and families have been disproportionately adversely affected by the Covid-19 pandemic and associated restrictions (Marmot et al., 2020; Best Beginnings, 2020). Babies in Lockdown (Best Beginnings, 2020) reported that 68% of parents felt their ability to cope with their pregnancy or baby had been affected by the pandemic, and a third believed that their baby’s interaction with them had changed.
Many families with lower incomes, from Black, Asian and minority ethnic communities and young parents have been hit harder by the COVID-19 pandemic. This is likely to have widened the already deep inequalities in the early experiences and life chances of children across the UK. (Best Beginnings, 2020: 9)
Research Study
Public Health Scotland has worked with the PIMH-PB to evaluate their programme of work and support the analysis of existing data held in the Child Health Surveillance Programme (CHSP), Family Nurse Partnership (FNP) records and maternity and mental health records (SG, 2021).
In keeping with this approach, Galloway et al. (2021) assessed the level of need for a designated infant mental health service in one Scottish Health Board area, population 655,000, comprising both urban and rural areas. Administrative data was explored at health board, local authority, and locality level about infant and parental vulnerabilities associated with the service criteria, which were to provide a service for infants (conception – 36 months) with:
- complex and significant needs in relation to parental mental health such as perinatal mental illness, substance or alcohol misuse, significant parental historical trauma, domestic abuse
- significant infant mental health disorder and development difficulty in infancy.
To assist with identifying local population needs, the report presented data collected by services but generally not publicly available especially at a detailed level, for example, data collected through routine inquiry undertaken within universal maternity and health visiting pathways and through child protection processes. It also included referrals, admissions and outcome data routinely collected by specialist perinatal services.
It was recognised that these figures may have understated the size of this population. Skovgard (2010) found the prevalence of serious mental health disorders in 18-month-old infants in the general population to be 16% in a large cohort longitudinal general population Danish epidemiological study. Predictors of these serious mental health disorders in 18-month-olds were identifiable at 10 months through a Health Visitor general population screening programme.
This Paper
Where the available data permits, this paper presents the results of an analysis of risks and concerns, and use of services, as these relate to the socioeconomic circumstances of families.
Methodology
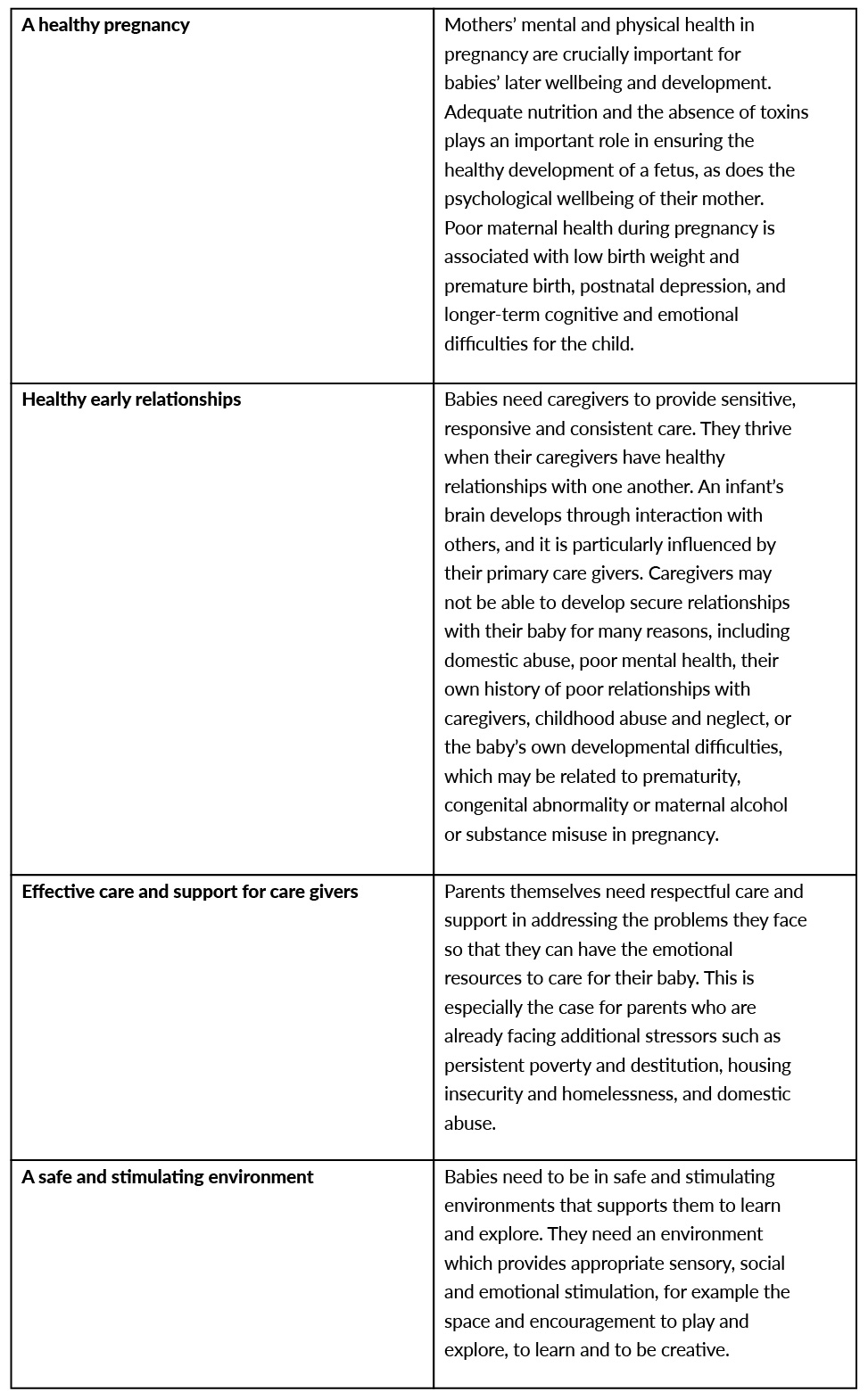
The data collection framework was based on the four key requirements (domains) for a healthy and safe start in life: a healthy pregnancy, healthy early relationships, effective care and support for caregivers, and a safe and stimulating environment which are described in Table 1 (Galloway et al., 2014). The need for an Infant Mental Health service might also be indicated by signs of concern in these areas or concerns about child protection or development. When these requirements are absent or compromised by family circumstances, the potential for mental health and developmental difficulties is increased.
Table 1. Key requirements for a healthy and safe start.
Data relating to these four domains, where available, was sourced from statutory agencies and comprised administrative data routinely recorded and collated by universal and specialist services. In addition, statutory child protection data was sourced indicating infants’ experience of harm. In terms of limitations, little or no data is available in relation to the quality of care for caregivers and the home and family environment. Another main limitation is the lack of insight into complexity; individual infants may be subject to multiple factors or counted multiple times in some datasets.
Disclosure to a professional is often difficult and self-report data may not be reliable. The picture presented by child protection figures is a partial one. Families where there were concerns about care giving below the threshold for statutory intervention, may not have been detected.
The Scottish Index of Multiple Deprivation (SIMD) (SG, 2020), an area-based measure of relative deprivation, was used. The most deprived SIMD income quintiles are where there are large numbers of people living at subsistence level. In this system, quintile 1 (Q1) refers to the area with highest income deprivation.
The health board comprises two local authorities, with ‘area N’ having significantly more deprivation than ‘area S’. Analysis looked at findings in each area in relation to the requirements for a healthy and safe start, and SIMD categorisation. It was collected over 4 years; the data reported here is for the year 2018/19, for the calendar year 2019, or as a 3 to 4 year average.
Results
This section presents a broad overview of general population data followed by a report of key findings by domain.
Broad Numbers
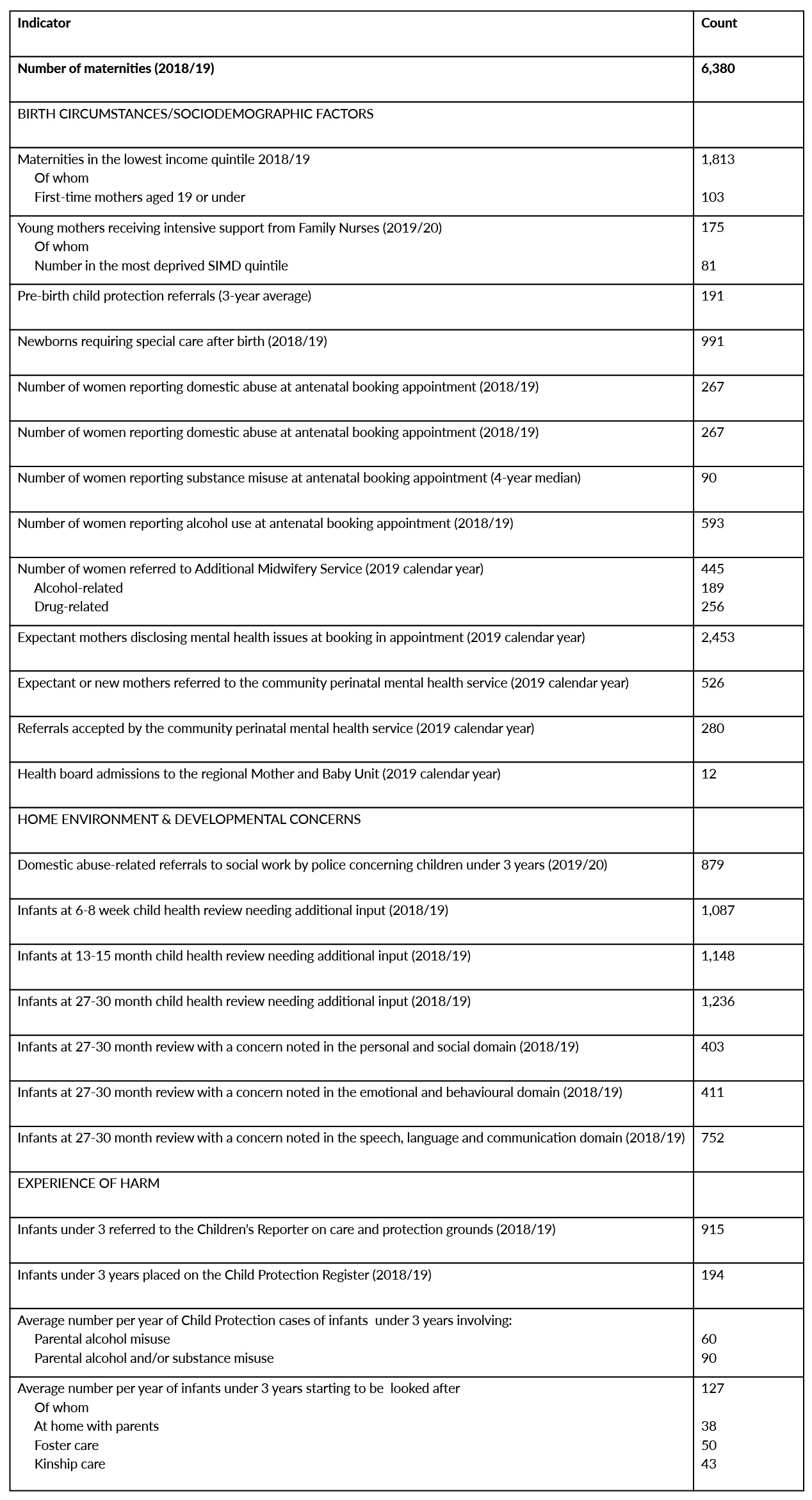
Table 2 shows information about the size of the population of infants whose life circumstances may undermine what they need for a healthy start, and whose odds of experiencing significant mental health disorders and development difficulties during the first 36 months of life are elevated.
Table 2. Broad Numbers (Infant and Family Population Statistics).
Key Findings
Domain 1: A Healthy Pregnancy
28% of all maternities were to mothers in SIMD Q1; this was higher in area N (32%) and lower, 22.5% in area S. In area N, almost one half (48%) of all maternities to young mothers under 20 years of age were in the most deprived income quintile.
Despite the overall decline in teenage pregnancies nationally, the gap between the most and least deprived areas has grown. The rate in the most deprived quintile in area N was 14.1 compared to 5.8 per 1,000 in the least deprived quintile. In area S the rate was 11.3 compared to 3.1 per 1,000. Family nurses provide support to young mothers, and their data provides an indication of the level of need, but only in relation to mothers who meet service criteria, based on age, first-time motherhood, and vulnerability. There remains a question about how much unmet need for intensive support exists, including for those having second and subsequent pregnancies. 46% of young mothers supported by Family Nurses belonged to SIMD Q1, and 77% of mothers and babies supported lived in the two most deprived areas.
3.1% of expectant mothers in SIMD Q1 reported substance misuse at ante-natal booking compared to 1.8% of all maternities. Reported alcohol use was highest in the least deprived area. There were an average of 90 child protection cases involving under 3’s, in which parental alcohol/substance misuse was involved.
On average 36% of women annually disclosed mental health issues during their booking-in appointment. Maternity data was cross-checked with data about acute psychiatric inpatient admissions in the 10 years before the date of delivery. Most of those identified lived in area N.
Referrals to the specialist perinatal mental health service varied across localities with a high rate of accepted referrals in the area of least deprivation, and low rates in the most deprived localities.
A higher percentage of newborns receive neonatal care compared with other health boards (15.4% compared with 11.1% in Scotland overall). In most localities the percentage is significantly higher for those in SIMD Q1, compared to the area as a whole, with around 40% of all babies from 3 deprived localities in area N being admitted.
Domain 2: Healthy Early Relationships
On average 4-5% of women reported domestic abuse at their antenatal booking, with a higher percentage reported in area N (5-7%). The presence of children under 3 years of age at domestic abuse incidents is reported by police to social work services. There were 879 referrals in 2019/20, with the number of incidents in area N being almost twice that in area S.
Domain 3: Effective care and support for caregivers
Data was not available to support the exploration of this domain.
Domain 4: A Safe and Stimulating Environment
A health needs assessment of children experiencing homelessness in area N was conducted by Campbell (2019). It found that a significantly higher proportion of children aged 0-5 years are present in households presenting as homeless, compared to the general population of area N, and that under-fives represented 38.9% of all children in homeless households, but 29.9% of the child population.
At the 27-30 month health check conducted by health visitors, infants in homeless households had significantly higher rates of any concern. Attendance at A&E for young children (<5 years) in homeless households was 31.9% higher than for the wider cohort.
Signs of Concern
Health visitors provide each child with a developmental review at age 6-8 weeks, 13-15 months, and 27-30 months. Infants are allocated ‘additional’ status if significant concerns are identified requiring sustained additional input. In 2018/19 over 1,000 infants at each of the three key child health reviews needed additional input to meet their health or developmental potential. Across the three reviews, a total of 3,471 infants and their carers required additional input. Proportionately more were in SIMD Q1. However, the percentage of infants allocated additional status overall was higher in area S than area N, despite deprivation levels being greater in the latter.
Those living in the most deprived areas made greater use of unscheduled care than those in the least deprived areas. The rate of A&E attendances in SIMD Q1 in area N was 349.3 per 1,000 compared with 275.2 per 1,000 in the least deprived quintile. Out-of-hours medical attendances by children aged 0-3 years were also related to the level of deprivation.
An average of 191 infants each year were subject to pre-birth child protection referrals. Just under two-thirds of these (63%) were in area N.
Discussion
In this study, the analysis of routinely recorded data held at national and local level provided an insight into inequality and its effects on infant mental health outcomes. The data reflects the services from which it is drawn, many of which are woman- or infant-focussed. As a result, information about fathers and the wider family was not captured. Limited use was made of data linkage, to investigate the psychiatric history of new mothers and the health of young children in homeless households. This has untapped potential.
The study confirms that many parents have difficulties in their lives, and a significant number of infants have experiences that can compromise their wellbeing and development. The complex interplay between these factors merits further investigation. A clear social gradient runs through the data and provides evidence that the structural inequalities in society may predetermine unequal developmental outcomes for infants. The analysis helps highlight the relative risks of experiencing adversity, which are more likely to be experienced by infants living in socioeconomically deprived areas. However, concerns can arise unexpectedly after birth in all families if, for example, an infant is born prematurely or has significant developmental problems. Yet there are also strong social gradients for the occurrence of prematurity and neurodevelopmental problems.
The access to some services for parents in socioeconomically deprived areas appears to be challenging. This is best illustrated by the rate of referrals to perinatal mental health services which was higher in one of the least deprived areas than in more deprived localities. However, expectant mothers in the most deprived areas were more likely to have had an acute psychiatry inpatient admission in the previous 10 years, to be under 25, and to have a history of substance use.
There is a social gradient relating to substance misuse; these expectant mothers are concentrated in the most deprived SIMD quintiles. Consideration should be given to both prevention and referral to specialist services for all those affected.
Expectant mothers in the least deprived income quintiles were more likely to report alcohol consumption in pregnancy or the period immediately before conception. Alcohol is damaging to fetal development and public health initiatives to address this should be targeted at all women of child-bearing age, with interventions being available to all women.
Alcohol or substance use by expectant or new mothers may be associated with spouses’ or partners’ use. Enquiries by midwives, obstetricians, health visitors and others are likely to be limited to the expectant mother. A systems approach would support wider enquiry into the circumstances of those beyond the mother-infant dyad, especially as both are associated with child protection referrals.
There is a clear relationship between SIMD category and admission to the neonatal unit. The rates for the total population were generally around 20% but elevated to 40% in 3 of the most deprived localities. It is concerning that so many newborns experienced a period of separation at a crucial time for the development of the mother-infant relationship.
17% of infants who received a child health review at 27-30 months had concerns identified, with a higher proportion being in the most deprived areas. A higher percentage in area S received ‘enhanced care’. Social gradient trends were also evident for A&E and out-of-hours attendances by infants and, as with concerns about development, had a strong association with homelessness.
In practice, rates of intervention depend upon many different factors. These include the ethos and approach to delivering services, service criteria, and factors that may vary across localities such as awareness of the importance of infant mental health, the knowledge and skills within teams of practitioners, the capacity for outreach, and the quality and consistency of relationships locally. Does the presence of multiple difficulties, some of which will be difficult to mitigate, discourage midwives and health visitors from providing more intensive input or making specialist referrals? An obvious exception might be referral to Family Nurse Partnership. The characteristics of those seen by family nurses show that as well as being young, mothers often experience multiple and interrelated difficulties, with a majority residing in the most deprived areas. However, in relation to the provision of enhanced input or referral to specialist services there does appear to be evidence of an inverse care law that is worthy of further exploration.
A deeper understanding of the local factors which might ameliorate or enhance the risks to the mental health of children and their parents and carers has the potential to inform both prevention and specialist service provision. Investment in public health interventions in disadvantaged areas may help to mitigate some of the consequences of adversity while the provision of targeted specialist perinatal and infant mental health services may alleviate distress and disorder, preventing later poor outcomes for infants.
References
Best Beginnings, Home-Start UK & the Parent Infant Foundation (2020). Babies in Lockdown: listening to parents to build back better. https://www.bestbeginnings.org.uk/news/the-babies-in-lockdown-report
Campbell, R. (2019). A health needs assessment of children experiencing homelessness in Lanarkshire. https://www.isdscotland.org/
Galloway, S., Haynes, A., & Cuthbert, C. (2014). An unfair sentence. All babies count. London: NSPCC
Galloway, S., Minnis, H., & McFadyen, A. (2021). Assessing the Need for an Infant Mental Health Service in NHS Lanarkshire. https://www.nhslanarkshire.scot.nhs.uk/download/infant-mental-health-report/
Marmot, M., Allen, J., Goldblatt, P. et al (2020). Build Back Fairer: The COVID-19 Marmot Review. http://health.org.uk/publication/COVID-19impactinquiry
Marryat, L., & Frank, J. (2019). Factors associated with adverse childhood experiences in Scottish children: a prospective cohort study. https://bmjpaedsopen.bmj.com/content/3/1/e000340
McFadyen, A. (2021) Wellbeing for Scottish Wee Ones: developing infant mental health systems in Scotland. Infant Observation, 24, 139-151. https://doi.org/10.1080/13698036.2021.1996909
Scottish Government (2018). Fairer Scotland Duty: interim guidance for public bodies. https://www.gov.scot/publications/fairer-scotland-duty-interim-guidance-public-bodies/
Scottish Government (2019a). Programme for Government. http://www.gov.scot/publications/protecting-scotlands-future-governments-programme-scotland-2019-2020/
Scottish Government (2019b). Getting it right for every child (GIRFEC) update: October 2019. http://www.gov.scot/publications
Scottish Government (2020). Scottish Index of Multiple Deprivation. https://www.gov.scot/collections/scottish-index-of-multiple-deprivation-2020
Scottish Government (2021). Perinatal and Infant Mental Health Programme Board Evaluability Assessment. https://www.gov.scot/publications/evaluability-assessment-scottish-governments-perinatal-infant-mental-health-programme/
Shonkoff, J. P., Slopen, N., & Williams, D. R. (2021). Early childhood adversity, toxic stress, and the impacts of racism on the foundations of health. Annual Review of Public Health 42:115-134. https://www.annualreviews.org/doi/full/10.1146/annurev-publhealth-090419-101940#_i2
Skovgaard, A. (2010). Mental health problems and psychopathology in infancy and early childhood. An epidemiological study. Danish Medical Bulletin, 57:1-30.
The Promise Scotland (2020). https://thepromise.scot
Tomlinson, M. (2015). Infant mental health in the next decade: a call for action. Infant Mental Health Journal, 36:538-541.
Treanor, M. C. (2020). Child poverty. Aspiring to survive. Bristol: Policy Press.
WHO (2018). Nurturing care for early childhood development. https://apps.who.int/iris/bitstream/handle/10665/272603/9789241514064-eng.pdf
Authors
Galloway, Susan,
Senior Policy Researcher,
NSPCC Scotland
Minnis, Helen,
Professor of Child and Adolescent Psychiatry,
Institute of Health and Wellbeing, University of Glasgow
McFadyen, Anne,
Consultant Child and Adolescent Psychiatrist, Infant Mental Health Lead, Perinatal Mental Health Network Scotland, and
Chair, Scottish Government Infant Mental Health Implementation and Advisory Group








