Abstract
The Department of Child Psychiatry of the Tampere University and University Hospital participated in a European multicentre study, that contrasted the effects of specially trained primary care nurses on newborn and parent-infant relationship outcomes in contrast to regular care delivery nursing practices. In the baseline measurement period, mothers receiving the intervention had more mental health problems and were poorer in their interaction with their infants than were mothers in the comparison condition. At the two year outcome measurement positive changes in Intervention Group mothers mental health and interaction behaviour were seen, and there were no significant differences in child behavior problems between the Intervention and Comparison Groups. In the five-year Finish follow-up there again were no significant differences in the child behavior problems between the two groups. This suggests that the positive changes gained during the two-year long European intervention study were maintained through the additional Finish follow-up period, but no evidence of further improvement in the children was seen.
Introduction
Healthy development of a child is dependent on biological, psychological and social factors. Infants are born with both biologically determined capacities and urge to participate in human interaction (Emde, 1983; Zeedyk, 1998; Trevarthen & Aitken, 2001). Early parent-infant interaction provides the contextual environment necessary for infants to develop. The quality of parent-infant interaction is affected by the qualities and behaviour of both. Normally parents are sensitized and attuned to meet the needs of their newborn (Emde, 1983; Brazelton & Cramer, 1990), but psychological distress, mental illnesses and drug and alcohol abuse have been shown to impair their ability to engage and interact with their infants in a satisfying way (Murray, Fiori-Cowley, Hooper, & Cooper, 1996; Zeanah, Boris, & Larrieu, 1997; Riordan, Appleby, & Faragher, 1999). Repetitive unsatisfying mother-infant interactions may have long-term consequences for the child, affecting the quality of attachment (Crittenden, 1995; Teti, Gelfand, Messinger, & Isabella, 1995) and restricting the child’s cognitive and socio-emotional development (Murray et al., 1996; Crockenberg & Leerkes, 2000; Carter,Garrity-Rokous, Chazan-Cohen, Little & Briggs-Cowan, 2001; Luoma et al., 2001). Since early parent-infant interaction affects the development of an infant (Nelson & Bosquet, 2000; Schore, 2001), it would seem reasonable to try to detect possible problems in the parent-infant interaction and intervene in early infancy.
Prevalence rates of mental health problems in children have been widely studied, and it has been estimated that 12-20 per cent of children suffer from these problems (Anderson, McGee & Silva, 1987; Ghaffer et al., 1996; Offord et al., 1987; Bird, 1996; Puura, 1998). Epidemiological studies on prevalence of mental health problems in younger children are still rare. One of the recent studies by Skovgaard et al. (2007) reported prevalence rates of 4.2% for disorders of affect, reactive attachment and adjustment, and prevalence rate for 8.5% for parent-infant relationship disorder in a sample of 18-month-old infants. Briggs-Gowan and colleagues (2001) found in their community sample of 1,279 children aged one and two years that the percentage of 2-year-olds with CBCL/2-3 scores in either clinical or sub clinical range, was 6.7% for internalizing problems.
Because for some children problems seem to emerge quite early, and because of relative stability of mental health problems during childhood and adolescence (Pihlakoski et al., 2006), the need for preventive interventions is evident. Currently there is evidence that interventions taking place in the perinatal period are most effective, even with high risk groups like prematurely born infants and families with multiple problems (Aronen, 1993; Barrera, Rosenbaum & Cunningham, 1986; Brooks-Gunn et al., 1994; Olds, Hill, Robinson, Song & Little, 2000; Zeanah, 1993). Educational interventions focused on giving guidance to parents have also yielded good results (McDonough 1995). In some studies the effects of early preventive intervention have been seen also in adolescence as less psychological problems (Aronen & Kurkela, 1996; Olds et al., 2000).
In Finland, children´s development is followed up in front line services, which for children under school-age means regular check-up visits in well-baby clinics. Each infant is seen monthly during the first year of life, twice in the second year of life and then once a year until the children enter school. The service is well accepted and used by 95% of families with small children, and provides a good framework for both supporting child development and screening for possible problems (Saarelma & Perheentupa, 1998). With increasing awareness of the importance of the early years of child development among Finnish health care professionals, the need to develop health promoting and preventive interventions usable in front line services became clear. For creating such an intervention the Department of Child Psychiatry of the Tampere University and University Hospital participated in a European multicentre study, The European Early Promotion Project (EEPP, Puura et al. 2002), with the support of the Finnish Ministry of Health and the National Centre for Research and Development of Social Welfare and Health.
The EEPP study was carried out simultaneously in Cyprus, Greece, Finland, Serbia and the United Kingdom. The EEPP aimed at giving nurses working in front line services better skills for supporting families where problems in early parent-infant interaction were found. The initial study lasted two years, and the outcome results from different countries have been reported elsewhere (Davis et al.,2005; Puura et al., 2005 ). For the Finnish sample the main outcomes of the EEPP were improved maternal mental health with less depressive episodes, less health problems in the children and increased maternal sensitivity in families who had been supported by the trained nurses (Davis et al., 2005; Puura et al., 2005).
In Finland we wanted to continue with a longer follow-up of the participating children and families. Our hypotheses was that the work done by the nurses trained in the EEPP would continue to have an effect on the families in the Intervention Group, resulting in less problem behaviours in children and better mental health in mothers. In this paper we will describe the results of the five-year follow-up of the Finnish sample of the EEPP.
Methods
First phase of the EEPP- study
The design, material and methods of the original EEPP-study have been described in detail in the main report (Puura et al., 2005), therefore only a short description is given here. The Finnish part of the EEPP study was carried out in Tampere, Finland. A group of 15 primary health care nurses working in well-baby clinics were trained to support mothers with new born babies and to intervene early should problems arise in the care of the infants. These Intervention Group nurses recruited mothers with new born babies to form the Intervention Group (n=93) for the study. A second group of 12 primary health care nurses without the additional training participated in the study (Comparison Group nurses) and recruited mothers with newborns to form the Comparison Group (n= 72). Nurses in both Intervention and Comparison Groups were asked also to assess the family´s need for support as they were recruited for the study.
The training of the Intervention Group nurses consisted of communication skills, infant development and early interaction, basic problem solving techniques and selected infant mental health intervention techniques, like modelling, open wondering (e.g. I wonder what your baby is needing when she cries like that?) and speaking for the infant (e.g. the nurse would say mimicking baby’s voice “mom pick me up, I want to be near you”). The skills learned in the training formed the basis for the intervention. The Intervention Group nurses contacted the mothers 4 weeks prior to giving birth and 6 to 8 weeks after delivery. If the mothers expressed any concerns or the Intervention Group nurses observed something worrying, the nurses invited distressed mothers to come to the well-baby clinic once or twice a week until the mothers felt more confident. During the visits the nurse would explore the worries with the mothers, encourage them to think about the infant’s behaviour and feelings, and support them in interacting with their infants. The interval between the visits gradually lengthened as the need for support diminished. The Intervention Group nurses also received regular supervision from a child mental health specialist during the two years of the EEPP intervention study.
The Comparison Group nurses received an introductory lecture on the design and purpose of the study, but no further training nor supervision. They were asked to contact the mothers they recruited for the study a month before the birth, 2 to 4 weeks after birth and then continue working with the mothers and infants as they normally would.
All families were assessed when the infants were 6-8 weeks old with a battery of instruments, including a semi structured interview, several questionnaires and parent-infant observation method by independent researchers during a home visit (see Puura et al., 2005). When the children were 2 years old the families (n= 139, 84% of the initial sample) were assessed with the same instruments as in the first assessment.
In addition to the measures used in the EEPP-study, the mothers of the Finnish sample also filled in the Child Behaviour Checklist as a part of the two-year assessment (CBCL; Achenbach 1992).
The follow- up from two to five years
The participating children had their 5-year birthday between March, 2003 and August 2004. The mothers were contacted by mail, and received an information letter about the study, the Child Behavior Checklist (CBCL) questionnaire, and a questionnaire with items concerning the health status of the child and his or her parents, information on child day care, and of the socioeconomic status of the family. All the questionnaires were marked with a research code to protect anonymity. Mothers also filled in an informed consent form, and sent all the forms back in a return envelope to an independent researcher.
Ninety two mothers returned completed CBCL questionnaires (53% of the original subjects and 67% of the subjects participating in the two-year assessment). The description of the study sample is given in Table 1. Families who did not participate in the 5 year follow-up did not significantly differ from those did in relation to socioeconomic factors or CBCL scores at the two year follow up at the T2.
The Ethical Committee of the Pirkanmaa Hospital District gave their permission for conducting the original study and the five-year follow-up.

Measures
The CBCL is an internationally used instrument designed to record children´s competencies and problems as reported by their parents. In this study the internalizing, externalizing and total problems scores were used as child outcome variables. The CBCL problem score is a sum score of problem items concerning withdrawal, somatic complaints and depressed/anxious symptoms, whereas the externalizing score is a sum score of problem items concerning delinquent and aggressive behavior. The raw scores of each sum score and the total score have been turned into T-scores. In the analyses we used two cut off points, 60 and 64, with 64 being the lower limit of the clinical range.
Statistical analyses
Differences between groups were tested with Fisher´s T-test and chi square when appropriate, and with Mann-Whitney U- test when variables were not normally distributed.
Results
Comparison of background variables between Intervention and Comparison Group
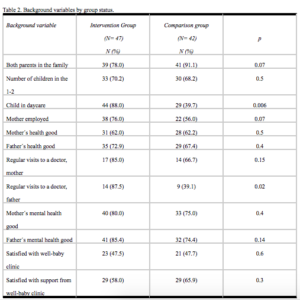
A comparison of background variables between the Intervention and Comparison Groups revealed three significant differences: A greater proportion of mothers (76%) in the Intervention Group worked outside home, compared to 50% of the Comparison Group mothers (p = 0.008); A greater proportion of children in the Intervention Group (88%) were in day care at the age of five, compared to 64% of the children in the Comparison Group (p= 0.006); and a greater proportion of fathers had regular visits to a doctor in the Intervention Group (87%) compared to 50% in the Comparison Group (p= 0.03).
Maternal reports of children´s symptoms
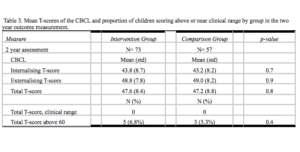
In the two year assessment with the CBCL no significant differences were found between Intervention and Comparison Group on how much problems or symptoms mothers reported about their children. None of the children scored in the clinical range in the total score of the CBCL at this time point. (Table 3). Five children in the Intervention Group and three in the Comparison Group scored above the cut off point of 60.
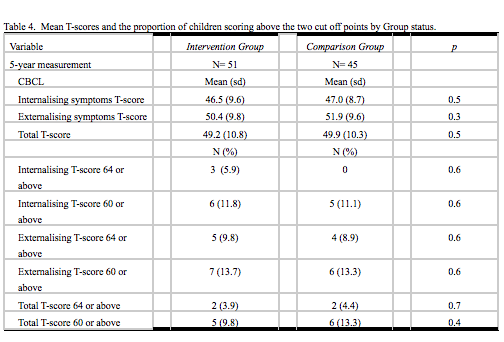
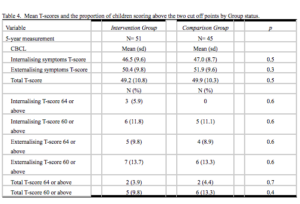
In the five-year follow-up no significant differences were found between the Intervention and Comparison Groups children in CBCL T-scores or in the proportion of children scoring above the two chosen cut off points of 60 and 64. However, in contrast to the two year assessment, at this time point four children scored in the clinical range (64 cut off) on the CBCL total problem behavior score (Table 4).
Discussion
The results reported in this paper pertain only to the Finnish sample within the larger EEEP two-year intervention study. The aim of the current study was to see whether the effects of the work of the trained nurses during the EEPP could be seen three years post intevention when the children were five years-old.
The main results in the Finnish sample in the outcome measurement of the EEPP-study, when the children were two year-old, were seen in maternal mental health, child health and in mother-infant interaction. Finnish mothers in the Intervention Group had had significantly less mild depressive episodes during the original study, and the children in the Intervention Group families had less chronic and severe health problems (Davis et al., 2005). Intervention Group mothers had become more reciprocal in their interaction with their infants, and offered more variation and stimulation for their infants, whereas no change was seen in the Comparison Group mothers (Puura et al. 2005). At the outcome measurement when the infants were two years-old the Intervention Group mothers were similar in interaction with their children as the Comparison Group mothers, although they had initially been significantly poorer (Puura et al., 2005).
In addition to the measures used in the EEPP, all mothers in the Finnish sample filled in CBCL forms as a part of the outcome measurement at two years. Perhaps reflecting the change in interaction behaviour of the Intervention Group mothers, there were no significant differences between maternal reports of the children´s symptoms in the Intervention and Comparison Group families in the CBCL.
In the five year follow-up measurement children in the Intervention Group were not different from Comparison Group children according to maternal reports. Contrary to our expectations, the Intervention Group children were not doing better than the Comparison Group children, meaning that there was no “sleeper effect” as has been seen in some intervention studies. The results may mean that the intervention had no impact on Intervention Group mothers’ perception of their children, at least not after the intervention had stopped when the children were two years old. Considering the initial situation where the Intervention Group mothers had poorer mental health and poorer interaction skills, the result can also be interpreted positively in the sense that the improvement seen in the Intervention Group mothers behaviour towards their children at two years was likely maintained, since the children were doing as well as the Comparison Group children. However, it seems that further improvement of the Intervention Group families would have needed continuing support.
Our hypotheses on better maternal mental health in the Intervention Group was also not supported. In the initial baseline measurement there were more mothers with mental health problems in the Intervention Group (Davis et al., 2005). In the five year follow-up mothers reported how they felt about their own and their spouses mental health. That there were no significant differences between the groups can be interpreted as a positive result of the two year long support from the well baby clinic nurses in the Intervention Group, but again no further improvement was seen after the support ended.
There are some limitations in this study that have to be considered. The size of the study sample was relatively small due to attrition, with 53% of the original subjects participating in the five-year follow-up. In follow-up studies attrition is inevitable due to people migrating to other areas in the country and to people being reluctant to participate in recurrent assessments. In this study a slight majority of the original subject participated in the five-year follow-up measurement. In attrition analyses the drop-out families were not significantly different from the participating families, and the remaining sample represents the original sample well.
Another limitation of the study is the use of questionnaires. Although the CBCL is internationally widely used and well valitated, the information it yields is limited compared to more intensive interview methods. The use of mothers as respondents limited the information to maternal reports, giving only mothers´perception of their children and of children´s fathers. Some of the questionnaires also had missing answers limiting the amount of data on these variables.
Conclusions
The initial intervention carried out in the EEPP-study supported mothers who were poorer in the interaction with their infants while it lasted and none of the mothers in the initially poorer Intervention Group reported their children having problems at clinical level at the age of two (Puura et al., 2005). However, no sleeper-effect was found after the end of the intervention, and in the five year follow-up the rate of children scoring above or close to clinical range had increased and was similar in the Intervention and Comparison Groups. In conclusion, it is likely that preventive interventions support better parenting under their duration but do not necessarily provide long-lasting help for parent-child problems.
For possible correspondence with the authors, please contact Kaija Puura, Department of Child Psychiatry, Tampere University Hospital, Po Box 2000, 33521 Tampere, Finland. Email kaija.puura@pshp.fi
References
Anderson J.C., McGee R. & Silva P. (1987). DSM- III disorders in preadolescent children. Archives of General Psychiatry, 44, 69-76.
Anthony B.J. Cognitive development in adolescence. In: Noshpitz J.D., Flaherty L.T., (Eds). Handbook of child and adolescent psychiatry. New York: John Wiley 1997;65-78.
Aronen, E.T. (1993). The effect of family counselling on the mental health of 10-11-year-old children in low- and high- risk families: A longitudinal approach. Journal of Child Psychology and Psychiatry, 34, 155-165.
Aronen, E.T. & Kurkela, S.A. (1996). Long-term effects of an early home-based intervention. Journal of the American Academy of Child and Adolescent psychiatry, 35, 1665-1672.
Barrera, M.E., Rosenbaum, P.L. & Cunningham, C.E. (1986). Early home intervention with low-birth-weight infants and their parents. Child Development, 57, 20-33.
Bates, J.E. (1988). Information on the Infant Characteristics Questionnaire. The Bates Infant Characteristics Questionaire.
Bayley, N. (1993). Bayley Scales of Infant Development. New York: Psychological Corporation.
Bird, H. (1996). Epidemiology of childhood disorders in a cross-cultural context. Journal of Child Psychology and Psychiatry, 37, 35-49.
Bradley, R. & Caldwell, B. (1979). Home Observation for measurement of the environment: A revision of the pre-school scale. American Journal of Mental Deficiency, 84, 235-244.
Brazelton, T.B. & Cramer, B.G. (1990). The earliest relationships. Reading, MA: Addison-Wesley.
Briggs-Gowan, M.J., Carter, A.S., Skuban, E.M., Horwitz, S.M. Prevalence of social-emotional and behavioral problems in a community sample of 1- and 2-year-old children. (2001). Journal of the American Academy of Child and Adolescent Psychiatry,40, 811-9
Brooks-Gunn, J., McCarton, C.M., Casey, P.H., McCormic, M.C., Bauer, C.R., Bernbaum, J.C., Tyson, J., Swanson, M., Bennee, F.C. & Scott, D.T. (1994). Early intervention in low-birth-weight premature infants. Results trought age 5-years from the Infant Health and Development Program. Journal of the American Medical Association, 272, 1257-1262.
Carter, A.S., Garrity-Rokous, E., Chazan-Cohen, R., Little, C., Briggs-Gowan, M. (2001). Maternal depression and comorbidity: predicting early parenting, attachment security, and toddler social-emotional problems and competencies. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 18-26.
Cowen, E.L., Pedro-Carroll, J.L. & Alpert-Gillis, L.J. (1990). Relationships between support and adjustment among children of divorce. Journal of Child Psychology and Psychiatry, 31, 727-735.
Crittenden, P.M. (1995). Attachment and risk for psychopathology: the early years. Developmental and Behavioral Pediatrics, 16, 12-16.
Crockenberg, S. & Leerkes, E. (2000). Infant social and emotional development in family context. In C.H. Zeanah (Ed.) Handbook of infant mental health. New York: The Guilford Press.
Davis, H., Dusoir, T., Papadopoulou, K., Dimitrakaki, C., Cox, A., Ispanovic-Radojkovic, V., Puura, K., Vizacou, S., Paradisiotou, A., Rudic, N., Chisholm, B., Leontiou, F., Mäntymaa, M., Radosavljev, J., Riga, E., Day, C. & Tamminen, T. (2005). Child and Family Outcomes of the European Early Promotion Project. International Journal of Mental Health Promotion, 7(1), 63-81.
Emde, R. N. (1983). Pre-representational self and its affective core. Psychoanalytic Study of the Child, 38, 165-192.
Ghaffer D., Fisher P., Dulcan M.K. et al. (1996). The NIHM Diagnostic interview Shedule for children version 2.3(disc2.3): Description, Acceptability, Prevalence rates, and performance in the MEGA study. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 865-877.
Luoma, I., Tamminen, T., Kaukonen, P., Laippala, P., Puura, K., Salmelin, R., Almqvist, F. (2001). Longitudinal study of maternal depressive symptoms and child well-being. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1367 -74.
McDonough S.C. (1995). Promoting positive early parent-infant relationships through interaction guidance. Child and Adolescent Psychiatric Clinics of North America, 4(3), 661-672.
Murray, L., Fiori-Cowley, A., Hooper, R. & Cooper, P. (1996). The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Development, 67, 2512-2526.
Nelson, C.A. & Bosquet, M. (2000). Neurobiology of foetal and infant development: implications for infant mental health. In Zeanah C.H., ed. Handbook of Infant Mental Health. New York: The Guilford Press, 2000.
Offord D.R., Boyle M.H., Szatmari P. et al. (1987). Ontario Health Study: II Six- month prevalence of disorder and rates of service utilization. Archives of General Psychiatry, 44, 832-836.
Olds, D.L., Hill, P., Robinson, L., Song, N., & Little, C. (2000). Update on home visiting for pregnant women and parents of young children. Current Problems in Pediatrics, 30, 109-141.
Pihlakoski, L., Sourander, A., Aromaa, M., Rautava, P., Helenius, H., Sillanpää, M. (2006). The continuity of psychopathology from early childhood to preadolescence: a prospective cohort study of 3-12-year-old children. European Child and Adolescent Psychiatry, 15(7), 409-17.
Puura, K. What children tell and adults notice-Child psychiatric disturbances among Finnish children. Acta Universitatis Tamperensis 605, 1998 Vammalan kirjapaino.
Puura, K., Davis, H., Papadopoulou, K., Tsiantis, J., Ispanovic, V., Rudic, N., Tamminen, T., Turunen, M.-M., Dragonas, T., Paradisiotou, A., Visacou, S., Day, C., Roberts, R., Cox, A. (2002). The European Early Promotion Project: A New Primary Health Care Service to Promote Children´s Mental Health. Infant Mental Health Journal, 23(6), 606-625.
Puura K., Davis H., Cox A., Tsiantis J., Tamminen T., Ispanovic-Radojkovic V., Paradisiotou A., Mäntymaa M., Roberts R., Dragonas T., Layiou-Lignos E., Dusoir T., Rudic N., Tenjovic L. & Vizacou S. (2005). The European Early Promotion Project: Description of the Service and Evaluation Study. International Journal of Mental Health Promotion, 7(1), 17-31.
Puura K., Davis H., Mäntymaa M., Tamminen T., Roberts R., Dragonas T., Papadopoulou K., Dimitrakaki C., Paradisiotou A., Vizacou S., Leontiou F., Rudic N., Miladinovic T. & Radojkovic A.. The Outcome of the European Early Promotion Project: Mother–Child Interaction. International Journal of Mental Health Promotion, 7(1): 82-94.
Riordan, D. Appleby, L. & Faragher, B. (1999). Mother-infant interaction in postpartum women with schizophrenia and affective disorders. Psychological medicine, 29, 991-995.
Saarelma, O., Perheentupa, J. (1998) Neuvola lasten terveyden edistäjänä. Duodecim, 114:1065-1069.
Schore, A. (2001). The effects of early relational trauma on right brain development, affect regulation, and infant mental health. Infant Mental Health Journal, 22 (1-2), 201-269.
Skovgaard A.M., Houmann T., Christiansen E., Landorph S., Jørgensen T.; CCC 2000 Study Team, Olsen E.M., Heering K., Kaas-Nielsen S., Samberg V., Lichtenberg A. (2007). The prevalence of mental health problems in children 1½ years of age – the Copenhagen Child Cohort 2000. Journal of Child Psychology and Psychiatry, 48, 62-70.
Stern, D.N. The Interpersonal World of the infant. A view from psychoanalysis and developmental psychology. New York: Basis Books 1985.
Teti, D.M., Gelfand, D.M., Messinger, D.S., Isabella, R. (1995). Maternal depression and the quality of early attachment: an examination of infants, preschoolers, and their mothers. Developmental Psychology, 31, 364-376.
Trevarthen, C. & Aitken K. J. (2001). Infant intersubjectivity: Research, theory, and clinical applications. Journal of Child Psychology and Psychiatry, 42, 3-48.
Zeanah, C.H., Boris, N.W., & Larrieu, J.A. (1997). Infant development and developmental risk: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 165-178.
Zeanah, C.Z. (Ed.) (1993). Handbook of infant mental health. New York: Guilford.
Zeedyk, M.S. (1998). Parent-infant interaction: interpreting meaning in infants’ actions. In C. A. Niven & A. Walker (Eds.), Current issues in infancy and parenthood. Butterworth Heinemann, Oxford.
Authors
Hermans, Virve, MD
Department of Child Psychiatry, Tampere University
Puura, Kaija, MD, PhD
Department of Child Psychiatry, Tampere University and University Hospital
Finland